Cynnwys
- Main findings
- Background
- Quality of care in the last 3 months of life
- Quality of care by place of death
- Quality of care by cause of death
- Quality of care by deprivation
- Quality of care by setting or service provider in the last 3 months of life
- Dignity and respect in the last 3 months of life
- Coordination of care in the last 3 months of life
- Relief of pain in the last 3 months of life
- Overall level of care in the last 2 days of life
- Support for relatives, friends or carers at the end of life
- Decision making at the end of life
- Preferences and choice at the end of life
- Sample information
- Questionnaire changes
- Uses and users of end of life care statistics
- Further information
- Acknowledgements
- References
- Background notes
- Methodoleg
1. Main findings
3 out of 4 bereaved people (75%) rate the overall quality of end of life care for their relative as outstanding, excellent or good; 1 out of 10 (10%) rated care as poor
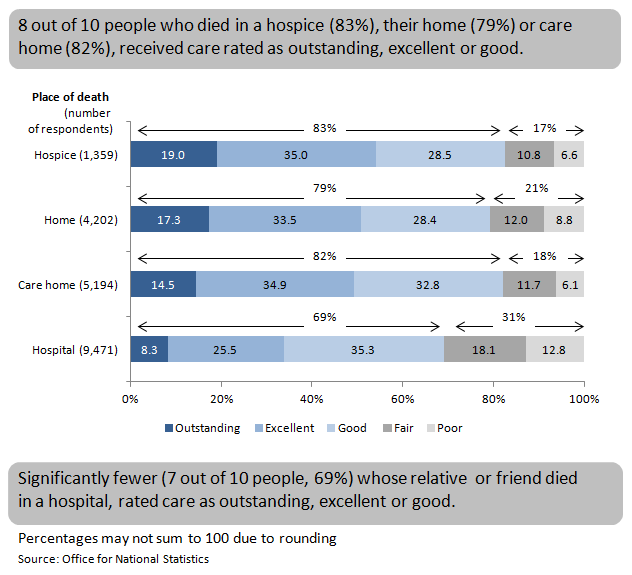
7 out of 10 bereaved people (69%) whose relative or friend died in a hospital, rated care as outstanding, excellent or good. This is significantly lower than outstanding, excellent or good ratings of care for those who died in a hospice (83%), care home (82%) or at home (79%)
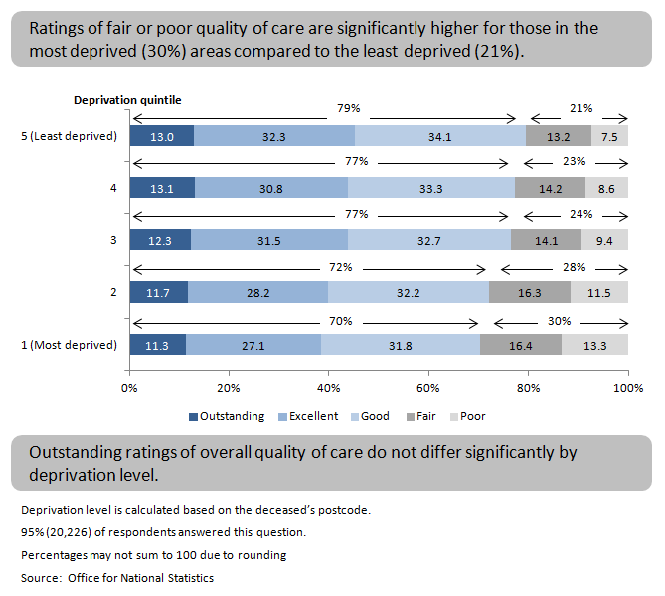
Ratings of fair or poor quality of care are significantly higher for those living in the most deprived areas (30%) compared to the least deprived areas (21%)
1 out of 3 (33%) reported that the hospital services did not work well together with GP and other services outside the hospital
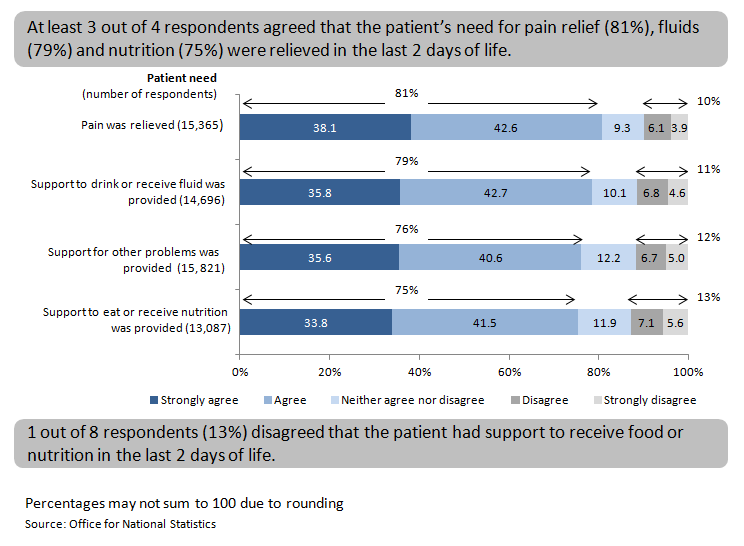
3 out of 4 bereaved people (75%) agreed that the patient’s nutritional needs were met in the last 2 days of life, 1 out of 8 (13%) responded that the patient did not have enough support to eat or receive nutrition
More than 5 out of 6 bereaved people (86%) understood the information provided by health care professionals, but 1 out of 6 (16%) disagreed they had time to ask questions with health care professionals
7 out of 10 (73%) respondents felt hospital was the right place for the patient to die, despite only 3% of all respondents stating patients wanted to die in hospital
2. Background
The National Survey of Bereaved People (VOICES, Views of Informal Carers – Evaluation of Services) collects information on bereaved peoples’ views on the quality of care provided to a friend or relative in the last 3 months of life, for England. The survey has now been run for 4 years and was commissioned by the Department of Health in 2011 and 2012, and NHS England from 2013. It is administered by the Office for National Statistics (ONS).
VOICES data provides information to inform policy requirements, including the End of Life Care Strategy, published by the Department of Health in July 2008. This set out a commitment to promote high quality care for all adults at the end of life and stated that outcomes of end of life care would be monitored through surveys of bereaved relatives ([Department of Health, 2008][1]). Recently, the Liverpool Care Pathway, which provided a protocol for end of life care, has received criticism ([Department of Health, 2013][2]). As a result, new questions were added to the VOICES survey in 2014 to measure changes in delivery of care while the Liverpool Care Pathway is replaced. Full details of the changes can be seen in the questionnaire changes section of the bulletin.
This statistical bulletin reports on the national results from the 2014 VOICES survey. This report includes findings from new survey questions, such as adequate provision of food and fluid in the last 2 days of life and quality of communication with carers. Full results can be seen in the [downloadable reference tables][3] (468.5 Kb Excel sheet) linked from this bulletin. NHS Area Team findings for the combined results of the 2012 and 2013 surveys can be seen in the bulletin: [National Survey of Bereaved People (VOICES) by NHS Area Team (England), 2012 – 2013][4] (ONS, 2015).
VOICES results are based on the opinions of relatives who rate the quality of care provided to their friend or relative. While 21,403 people responded to the survey, not all of the survey questions are relevant to, or answered by all respondents so some results are based on the answers from fewer people than others. Where relevant the number of respondents for a question is provided to aid interpretation. Further guidance on interpreting the results in this bulletin is provided in background notes 7 to 9.
[1]: https://www.gov.uk/government/publications/end-of-life-care-strategy-promoting-high-quality-care-for-adults-at-the-end-of-their-life (Department for Health, 2008" [2]: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/212450/Liverpool_Care_Pathway.pdf "Department of Health, 2013" [3]: http://www.ons.gov.uk/ons/rel/subnational-health1/national-survey-of-bereaved-people--voices-/2014/rft-1.xls "Reference table 1" [4]: http://www.ons.gov.uk/ons/rel/subnational-health1/national-survey-of-bereaved-people--voices-/by-nhs-area-team--england---2012-13/stb-national-survey-of-bereaved-people--voices-.html "National survey of bereaved people by NHS area team, 2012 to 2013"
Nôl i'r tabl cynnwys3. Quality of care in the last 3 months of life
Ratings of the overall quality of care across all services in the last 3 months of life were reported by most respondents (95%, 20,226 responses). Services included care provided by hospitals, care homes, hospices and care while at home from GPs and care services. Of all responders, 3 out of 4 (75%) rated care as outstanding, excellent or good, while 1 in 10 (10%) rated care as poor (see Figure 1).
Figure 1: Ratings of overall quality of care across all services in the last 3 months of life, England, 2014
Source: Office for National Statistics
Notes:
- Percentages may not sum to 100 due to rounding.
- 3 out of 4 (75%) rated the overall quality of care as outstanding, excellent of good. 1 in 10 rated the overall quality or care as poor.
- 95% (20,226) of respondents answered this question.
Download this chart Figure 1: Ratings of overall quality of care across all services in the last 3 months of life, England, 2014
Image .csv .xls4. Quality of care by place of death
The relatives of people who died in hospital rated overall quality of care significantly worse than any other place of death. Almost one third (31%) rated care in hospitals as fair or poor, compared to the lowest rate of 17% rating care as fair or poor in hospices. Respondents for approximately 8 out of 10 people who died in hospices (83%), care homes (82%) or their own home (79%) rated care as outstanding, excellent or good. Again, hospitals are significantly below this, with 7 out of 10 (69%) respondents rating care as outstanding, excellent or good (Figure 2).
Figure 2: Overall quality of care by place of death, England, 2014
Source: Office for National Statistics
Download this image Figure 2: Overall quality of care by place of death, England, 2014
.png (42.6 kB) .xls (27.1 kB)5. Quality of care by cause of death
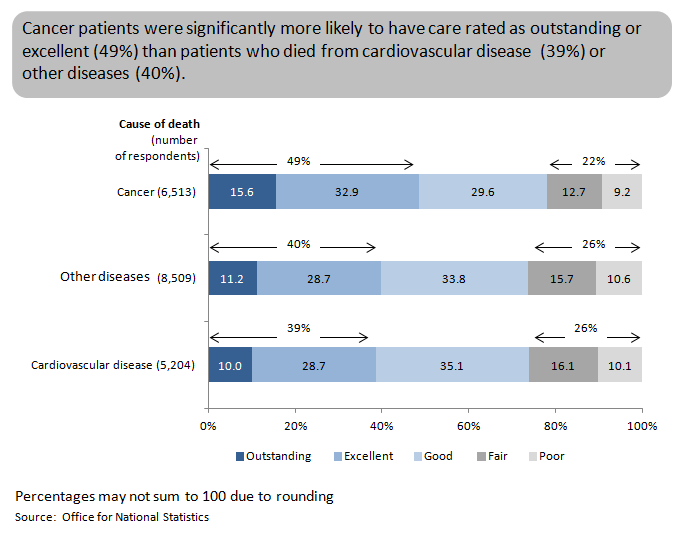
When looking at overall quality of care for different causes of death, outstanding, excellent and good ratings combined do not differ significantly for people rating the care of cancer patients (78%), cardiovascular patients (74%) or patients dying from other causes (74%). However, when examining the ratings for outstanding and excellent only, overall quality of care for cancer patients in the last 3 months of life is rated significantly higher than care for people dying from cardiovascular disease or other causes. Just under half (49%) of cancer patients had care rated as outstanding or excellent, compared with 39% of cardiovascular disease patients and 40% of people dying from other causes (see Figure 3).
Figure 3: Overall quality of care by cause of death, England, 2014
Source: Office for National Statistics
Download this image Figure 3: Overall quality of care by cause of death, England, 2014
.png (36.1 kB) .xls (26.6 kB)6. Quality of care by deprivation
A notable pattern of overall quality of care exists when considering the level of deprivation of the deceased. While there is no difference in the proportion of people rated as receiving outstanding care by deprivation level, there is an association between greater deprivation and ratings of poor care (see Figure 4). Significantly more people with the most deprived status have care rated as fair or poor (30%) compared to the least deprived group (21%). This echoes the finding from the VOICES by area deprivation bulletin (ONS, 2013a). Further details are available in the downloadable Reference Table 1 (468.5 Kb Excel sheet) , “Overall quality” tab.
Figure 4: Overall quality of care by deprivation quintile, England, 2014
Source: Office for National Statistics
Download this image Figure 4: Overall quality of care by deprivation quintile, England, 2014
.png (43.7 kB) .xls (27.1 kB)7. Quality of care by setting or service provider in the last 3 months of life
Respondents are asked to rate the quality of care within each setting that the patient was looked after in the last 3 months of life. Overall quality of care questions asked respondents to consider all aspects of care provided and rate them together, while in contrast, quality of care by setting or provider questions enabled respondents to rate specific care settings that the patient had experienced. These included rating care at home, in a hospital, in a care home or in a hospice and from specific care providers such as district nurses and health professionals who can respond to urgent needs outside normal working hours (urgent care providers). Quality of care by setting is measured on a 4 point scale from excellent to poor.
Quality of care rated as excellent was highest where care was provided by hospices (75%) and lowest where care was provided by urgent care services (26%). As seen in overall quality of care, approximately 1 in 10 people rated care provided by hospital doctors (9%) and hospital nurses (11%) and GPs (13%) as poor (see Figure 5).
Figure 5: Quality of care by care setting or provider in the last 3 months of life, England, 2014
Source: Office for National Statistics
Notes:
- Percentages may not sum due to rounding.
- This question is multi coded so the respondent can tick more than one option.
- 3 out or 4 people (75%)rated the care provided by hospice staff as excellent. 1 out of 4 people (26%) rated the care provided by urgent care services as excellent.
Download this chart Figure 5: Quality of care by care setting or provider in the last 3 months of life, England, 2014
Image .csv .xlsReference Table 1 contains results of quality of care ratings within each health care setting. Quality of care is significantly higher for people who died of cancer compared with cardiovascular disease or other causes. For cancer patients, hospice care was rated 81% excellent, district and community nurses 51% excellent, GPs 41% excellent and urgent care 29% excellent. See Reference Table 1 (468.5 Kb Excel sheet) ("Quality of care (3mnth)" tab).
Nôl i'r tabl cynnwys8. Dignity and respect in the last 3 months of life
One aspect of care measured was how much staff in different settings treated the patient with dignity and respect. Staff in hospices were most likely to be rated as always showing dignity and respect to the patient in the last 3 months of life (88% for hospice doctors and 85% for hospice nurses). Hospital staff received the lowest ratings of always showing dignity and respect. This was 59% for hospital doctors and 53% for hospital nurses. While dignity and respect from hospital nurses is lower than from doctors, it has increased significantly from 48% in 2011 to 53% in 2014 (see Figure 6).
Figure 6 presents information on how often the patient was treated with dignity and respect in the last 3 months by setting or service provider in 2014. Where settings are less likely to be rated as always treating patients with dignity and respect, such as care homes and hospitals, more people (roughly 1 in 4) rate that dignity and respect was given most of the time (care homes 28%, hospital doctors 25%, and hospital nurses 27%). 1 out of 5 people (21%) rate hospital nurses as only treating patients with dignity and respect some of the time or never, while GPs are significantly more likely to be rated as never treating patients with dignity and respect in comparison to all other settings (4%).
Figure 6: Dignity and respect by care setting or provider in the last 3 months of life, England, 2014
Source: Office for National Statistics
Notes:
- Percentages may not sum to 100 due to rounding.
- Hospice doctors and hospice nurses are significantly more likely to be rated as always treating patients with dignity and respect in comparison to other settings.
- 1 out of 5 people (21%) rate hospital nurses as only treatin patients with dignity and respect some of the time, or never.
Download this chart Figure 6: Dignity and respect by care setting or provider in the last 3 months of life, England, 2014
Image .csv .xlsAlways receiving dignity and respect from health care professionals is reported as higher for people who die of cancer than for patients dying of cardiovascular or other causes. This is significantly higher for cancer patients receiving care from hospice doctors and nurses as well as GPs and community nurses, compared to cardiovascular patients or patients with other diseases. Differences in dignity and respect shown to patients of different ages tend to be small and non significant. Further details of responses related to dignity and respect reported by the different care settings and care providers in the last 3 months and the last 2 days of life are provided (see "Dignity and Respect 3 months" and "Dignity and Respect 2 days" tables in reference table 1 (468.5 Kb Excel sheet) ).
Nôl i'r tabl cynnwys9. Coordination of care in the last 3 months of life
Two questions were asked about coordination of care. One question was asked in relation to those patients who had spent some or all of the last 3 months at home, about whether community services worked well together. Of the 47% (9,530) of people who responded to this question, 42% said that the services definitely worked well together (see Figure 7). This was significantly higher for people who died at home (55%) compared to those who died in a hospice (40%), hospital (35%) or care home (32%, see Reference Table 1 (468.5 Kb Excel sheet) "Coordination of care (3mnth)" tab). This provides support for the view that coordinated services in the community can enable people to die at home.
Figure 7: Coordination of care between care services in the last 3 months of life, England, 2014
Source: Office for National Statistics
Notes:
- Percentages may not sum to 100 due to rounding.
- 1 in 3 respondents (33%) reported the hospital services did not work well together with GP and other services outside of the hospital.
- 42% of respondents whose relative or friend had spent some or all of the last 3 months at home agreed that the care services defiantly worked well together.
Download this chart Figure 7: Coordination of care between care services in the last 3 months of life, England, 2014
Image .csv .xlsRespondents were asked to answer the second coordination of care question if the patient had spent some time in hospital in the last 3 months of life. This asked if hospital services worked well with the GP and other community services outside the hospital. Here, 46% (9,405) responded to the question (9,405 people) with 1 in 3 people (33%) reporting that services did not work well together. About 2 out of 3 (67%) said that the services definitely worked well together or worked well together to some extent. Statement 8 of the National Institute for Health and Care Excellence (NICE) quality standards for End of Life Care for Adults emphasises the importance of effectively coordinated care across all relevant settings (NICE, 2011). See “Coordination of care” table in Reference Table 1 (468.5 Kb Excel sheet) .
Nôl i'r tabl cynnwys10. Relief of pain in the last 3 months of life
Figure 8 presents results on how well pain was relieved during the last 3 months of life, by care setting. Questions on relief of pain were relevant only for certain patients. Where it was relevant, relief of pain was reported as being provided "completely, all of the time" most frequently for patients in hospices (64%) and least frequently for those at home (18%). Almost 1 in 13 (8%) of people cared for at home did not have their pain relieved at all. Pain relief does not vary significantly between cause of death or age of death at home, in a hospital or in a hospice. In care homes, more than 2 out of 5 (22%) cancer patients had their pain relieved all of the time, which was significantly higher than people who died from cardiovascular disease (13%) or other causes (15%). For further information, see "Relief of pain 3 months" and "Relief of pain 2 days" tables in Reference Table 1 (468.5 Kb Excel sheet) .
Figure 8: Relief of pain by care setting in the last 3 months of life, England, 2014
Source: Office for National Statistics
Notes:
- Percentages may not sum to 100 due to rounding.
- Pain was reported being relieved 'completely, all of the time' most frequently for patients in hospices (64%) and least frequently for those at home (18%).
- Almost 1 in 13 (8%) of people cared for at home did not have their pain relieved at all.
Download this chart Figure 8: Relief of pain by care setting in the last 3 months of life, England, 2014
Image .csv .xls11. Overall level of care in the last 2 days of life
In 2014, new questions were added to the VOICES questionnaire to understand the overall level of care given by health professionals in the last 2 days of life. These related to the respondent’s opinions on whether the patient was given adequate nutrition, fluid and pain relief in the last 2 days of life as well as how well the patient’s non medical needs were met. These questions were added to provide an indicator of how well needs are met at the end of life following the withdrawal of the Liverpool Care Pathway.
Figure 9 shows that between 75% and 81% of cases, relatives agreed or strongly agreed that patients had adequate support to relieve thirst, hunger, pain and other problems. This indicates that in at least 3 out of 4 cases, people’s primary needs are met at the end of life. Despite this, 1 in 8 respondents (13%) disagreed or strongly disagreed that the patient’s need for food or nutrition was met. A similar proportion (11%) disagreed that there was adequate support for the patient to receive fluids and 12% disagreed that other problems were supported. One in 10 (10%) disagreed that pain relief was sufficient in the last 2 days of life.
Figure 9: Overall level of practical care provided by health professionals in the last 2 days of life, England, 2014
Figure 9: Overall level of practical care provided by health professionals in the last 2 days of life, England, 2014
Source: Office for National Statistics
Download this image Figure 9: Overall level of practical care provided by health professionals in the last 2 days of life, England, 2014
.png (32.3 kB) .xls (27.1 kB)Other new questions asked about the emotional and practical support provided in the last 2 days of life. Similar proportions of people agreed or strongly agreed that the patient’s emotional needs were considered and supported (70%) and that the patient was cared for in the place they wanted to be (70%). Despite this, 1 in 7 people disagreed that these needs were met, with 15% disagreeing or strongly disagreeing that the patients emotional needs were supported or that they were cared for in the place they wanted to be (15%, see Figure 10).
Significantly fewer people agreed that support and consideration for spiritual and/or religious needs was provided in comparison to other needs. Only 60% of people agreed or strongly agreed that support for religious and/or spiritual needs was provided, although a higher proportion of people responded with neither agree or disagree than for any other question (25%). This may reflect that this is not an important factor for all patients, or that respondents do not expect this need to be supported by health care staff. The result that 33% of respondents to the survey ticked the additional "does not apply" option may further reflect this. Full results are available in Reference Table 1 (468.5 Kb Excel sheet) , “overall care (2 day)” tab.
Figure 10: Overall level of emotional care provided by health professionals in the last 2 days of life, England, 2014
Figure 10: Overall level of emotional care provided by health professionals in the last 2 days of life, England, 2014
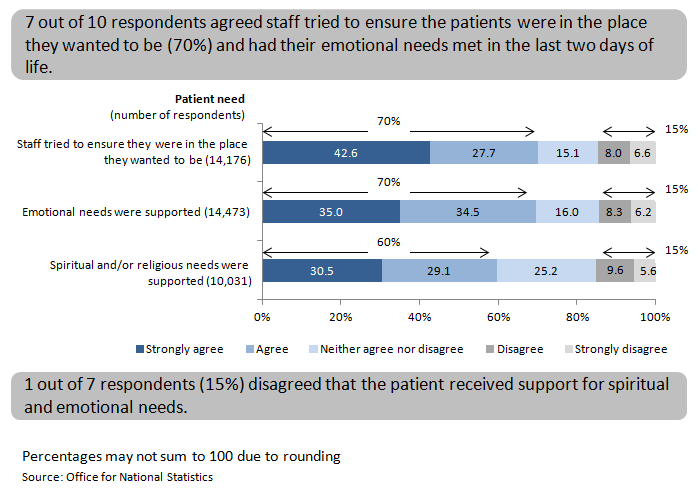
Source: Office for National Statistics
Download this image Figure 10: Overall level of emotional care provided by health professionals in the last 2 days of life, England, 2014
.png (28.4 kB) .xls (27.1 kB)12. Support for relatives, friends or carers at the end of life
In 2014, new questions were asked about the quality of communication between relatives, friends or carers and health care professionals in the last 2 days of life. The majority of people responded agree or strongly agree to the questions “we understood the information given to us” (86%), “we were kept informed of his/her condition and care” (79%), “we had enough time with staff to ask questions and discuss his/her condition and care” (76%) and “we had a supportive relationship with the health care professionals” (74%, see Figure 11). In contrast, between 7% and 16% disagreed or strongly disagreed with these statements.
Figure 11: Quality of communication with health care professionals in the last 2 days of life, England, 2014
Figure 11: Quality of communication with health care professionals in the last 2 days of life, England, 2014
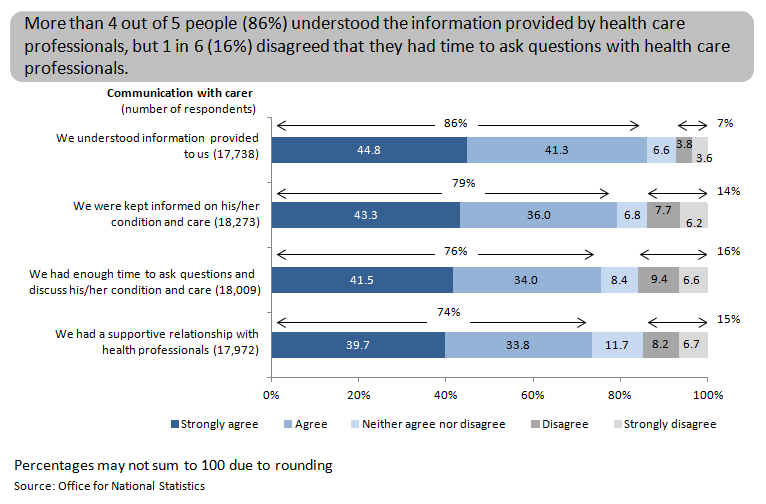
Source: Office for National Statistics
Download this image Figure 11: Quality of communication with health care professionals in the last 2 days of life, England, 2014
.png (31.1 kB) .xls (27.6 kB)Reference Table 1 (468.5 Kb Excel sheet) (“communication (2 day)” tab) presents these results broken down by different categories. When comparing quality of communication results by place of death, respondents whose friend or relative died in hospital were significantly less likely to agree or strongly agree that they were kept informed of the patient’s condition (74% compared to the next lowest of 82% at home), that staff had enough time to discuss the patient’s condition and care (68% compared to the next lowest of 80% at home), or that the health professionals had a supportive relationship with the carer (66% compared to the next lowest of 79% in a care home).
Significantly more relatives of people treated in hospital than other settings reported poor communication with health professionals. As many as 1 in 5 people disagreed or strongly disagreed that they were able to discuss the patient’s condition with staff (22%), that they had a supportive relationship with staff (20%) or that they were kept informed of the patient’s condition (19%). Significantly more people whose relative or friend died in hospital also did not understand the information provided to them (10%) in comparison to other settings.
Notably, respondents aged under 60 are significantly less likely to answer positively to these questions than those aged over 60. For instance, those aged under 60 agreed or strongly agreed that they had enough time to ask questions and discuss the patient’s condition less than those aged over 60 (71% compared to 80% respectively).
Other questions on the survey asked about the support the respondent and family of the deceased received and whether they were dealt with sensitively. More than half of respondents to these questions (59%) said that they had definitely been given enough support at the time of the death. A further 27% said that they had to some extent.
When asked whether they had talked to anyone from any support services since the death, most respondents reported that they had not, and did not want to (66%). However, 20% said that they had not, but would have liked to. This was significantly higher for female respondents (23% versus 16% for males) and younger respondents (25% for under 60 years and 16% for those 60 years and over).
The National Institute for Health and Care Excellence (NICE) quality standards for End of Life Care for Adults (Statements 7 and 14) focuses on the importance of sensitive communication to those closely affected by death and the need to offer timely support "appropriate to their needs and preferences" (NICE, 2011). Further information is presented in the “Support for carer 3 months” and “Support for carer 2 days” tables in Reference Table 1 (468.5 Kb Excel sheet) .
Nôl i'r tabl cynnwys13. Decision making at the end of life
Most people (97%, 20,705) responded to the question of whether decisions were made about care which the patient would not have wanted. Of these, almost 1 out of 5 (19%) respondents said that decisions were made about the patient’s care, which the patient would not have wanted. Approximately 3 out of 5 (61%) respondents said that no decisions were made that the patient would not have wanted.
Respondents reported that they believed the majority of patients (86%) were involved in decisions about their care as much as they wanted (62% of the sample (13,314 people) responded to this question). Statement 3 of the National Institute for Health and Care Excellence (NICE) quality standards for End of Life Care for Adults, emphasises the importance of people approaching the end of life feeling satisfied that they have been able to discuss, record and review their needs and preferences and take a role in planning and decision-making, if they would like to do so (NICE, 2011). Further details about decision making around care are reported in the “Patients Needs and Preferences 3 Months” tables in Reference Table 1 (468.5 Kb Excel sheet) with results presented by cause of death, place of death and age at death.
Nôl i'r tabl cynnwys14. Preferences and choice at the end of life
Respondents were asked if the patient had expressed a preference for where they would like to die and asked to state where this was (for instance, at home, in a hospice etc.). The majority believed the deceased had wanted to die at home (82%), 8% said they wanted to die in a hospice, 6% in a care home, 3% in hospital and 1% somewhere else (see Reference Table 1 (468.5 Kb Excel sheet) , "priorities (3mnth)" tab). Previous VOICES evidence also shows that 54% of people died in their preferred place of death but only 4% of these died in hospital, indicating that this is not where people choose to die (ONS, 2015).
Respondents were asked if the patient had died in the right place and 99% of people who responded to the survey, answered this question (21,087). Figure 12 presents those who were believed to have died in the right place for their circumstance, by the place of death. This shows that in hospices and at home more than 9 out of 10 people (94% for each place) were believed to have died in the right place for them. This figure reduces to 73% for people dying in hospitals. Hospitals also have the highest proportion of respondents who felt the deceased did not die in the right place (16%) and respondents who were not sure if hospital was the right place for the deceased to have died (11%).
Figure 12: Did the patient die in the right place, by place of death, England, 2014
Source: Office for National Statistics
Download this chart Figure 12: Did the patient die in the right place, by place of death, England, 2014
Image .csv .xls15. Sample information
The sample for the 2014 VOICES survey was selected from the adult deaths registered between 1 January 2014 and 30 April 2014, which were extracted from our death registration database. Records were removed where cause of death and place of death were outside the criteria (see below), where the informant’s name and address was missing and where the informant was designated an official (See Background Note 4).
From the 135,880 deaths that were eligible for the survey, a stratified sample of 49,614 was drawn for the actual survey.
Informants were contacted between 4 and 11 months following the death, the recommended time for such surveys to balance the need for privacy and sensitivity during early bereavement while ensuring reliable recall about care provision (Hunt et al, 2011). The mailing period was also timed to exclude Christmas and the anniversary of the death. The VOICES-SF questionnaire was used: the Views of Informal Carers – Evaluation of Services (VOICES) short-form (see Background Note 3), which incorporated the new survey questions outlined in the questionnaire changes section of this report.
Sex of deceased
This was determined from information recorded on the death certificate.
- male (47% of the selected sample)
- female (53% of the selected sample)
Place of death
Deaths were excluded where the place of death was recorded as "Elsewhere", which includes external sites (such as roads or parks), public venues (such as shops or restaurants), work places and any other place which could not be identified to a specified location type. Location types that were included were grouped in the following way:
- home: the home of the deceased as reported on the death certificate. (23% of the selected sample)
- hospital: NHS and private (49% of the selected sample)
- care homes (including residential homes) (22% of the selected sample)
- hospices (6% of the selected sample)
In some cases, it may be appropriate to group residential homes with home, since these all describe the usual residence of the person. However, for the purposes of the 2014 VOICES survey, residential homes were grouped with care homes because the survey addresses the quality of care provided by staff.
Cause of death
All details relevant to the cause of death on the death certificate are coded using the International Statistical Classification of Diseases and Related Health Problems – Tenth Revision, or ICD–10 (WHO, 1992).
Deaths were excluded from the sampling frame where the underlying cause of death was accident, suicide or homicide (ICD–10 codes V01 to Y98 and U50.9). The following deaths were included where they were recorded as the underlying cause:
- cardiovascular disease (CVD): ICD–10 codes I00 to I99 (29% of the selected sample)
- cancer ICD–10 codes C00 to D48.9 (This includes benign neoplasms) (30% of the selected sample)
- other: ICD–10 codes A00 to R99 (excluding CVD and Cancer) (41% of the selected sample)
Age at death
Deaths of people aged under 18 years were excluded, leaving an age range of 18 to 110 years for the sample. Ages were split into 3 groups.
- under 65 years (12% of the selected sample)
- 65 to 79 years (28% of the selected sample)
- 80 years or older (60% of the selected sample)
This older age group becomes of greater importance as the number of older adults increases (ONS, 2014a), mortality rates fall (ONS, 2013b) and people live longer (ONS, 2014b).
Geographical spread
To ensure a geographical spread, death records were assigned to an NHS Area Team based on the postcode of usual residence of the deceased. In 2014, there were 25 NHS Area Teams covering the whole of England.
Response rates
Of the sample of 49,614 deaths, 21,403 completed responses were received from informants, giving a response rate of 43%. The overall response rate has reduced by 3% in comparison with the 2013 survey (ONS, 2014c). This is likely to be due to changes to the questionnaire, such as making the method to refuse to participate more explicit and a declining trend in survey response rates more widely.
Reference Table 1 (468.5 Kb Excel sheet) (“Response rates” tab) presents the response rates by characteristics of the deceased. Our mortality database contains the name and address of informants of the death and, in most cases, the relationship of the informant to the deceased. No further information about the informant was available so it was not possible to estimate response rates based on respondent details. Although the questionnaire is sent to the informant on the death certificate, they are encouraged to pass on the questionnaire to another family member if deemed more appropriate. In the questionnaire, respondents were asked their age, sex, ethnic group and relationship to the deceased. Where answers were provided, 61% of the sample were female, 56% aged over 60 and 97% were white.
Nôl i'r tabl cynnwys16. Questionnaire changes
The Liverpool Care Pathway provided a protocol for end of life care which has received criticism in a recent review (Department of Health, 2013). Following this review, the Leadership Alliance for the Care of Dying People was established to deliver improvements in end of life care (NHS England, 2013). The Leadership Alliance has published a commitment to priorities for improving care of the dying person, including improving communication between staff, the dying person and their carers, involving the dying person and their carers in decisions about their care and providing an individual plan of care to meet physical and psychological needs of the dying person (Department of Health, 2014).
The VOICES questionnaire has been developed to take account of these policy changes. New questions were developed in relation to provision of fluid, nutrition and other aspects of care at the end of life and the quality of communication with carers and support for their needs. These new questions were cognitively tested in spring 2014 and included in the 2014 VOICES survey. The results can be found within this bulletin in the sections Overall level of care in the last 2 day of life and Support for friends, relatives and carers at the end of life.
Cognitive testing of these new questions has also lead to small changes in existing parts of the questionnaire. These changes will ensure the questionnaire continues to provide policy relevant information and is easy for respondents to complete. A full comparison of the old and current VOICES survey is available here (144 Kb Excel sheet) and the male version (107.1 Kb Pdf) and female version (112.9 Kb Pdf) of the questionnaires can also be downloaded.
The policy changes in end of life care will affect the delivery of services, furthering the importance of continuing to monitor quality of care through surveys such as the National Survey of Bereaved People (VOICES).
Nôl i'r tabl cynnwys17. Uses and users of end of life care statistics
The National Survey of Bereaved People (VOICES) has a range of uses and users. The Department of Health commissioned this survey to follow up on a commitment made in the End of Life Care Strategy. The results of this survey will be used to inform policy decisions and to enable evaluation of the quality of end of life care in different settings, across different ages and different causes of death.
The Liverpool Care Pathway has provided a protocol for end of life care which has received criticism in a recent review (Department of Health, 2013). Following this review, the Leadership Alliance for the Care of Dying People has been established to provide improvements in end of life care (NHS England, 2013). VOICES statistics provide data which will enable the impact of end of life care policies to be monitored during this transitional period.
NHS England are taking this work forward. Quality of end of life care is 1 of the main areas in the NHS Outcomes Framework. This has relevance for Domain 2 "Enhancing quality of life for people with long-term conditions" and Domain 4 "Ensuring that people have a positive experience of care". Indicator 4.6 "Improving the experience of care for people at the end of their lives" uses data from VOICES to gather bereaved carers’ views on the quality of care in the last 3 months of life.
VOICES data is also used to support third sector activity, such as supporting lobbying campaigns to improve care at home, allocating charity resources and evaluating and comparing service provision across settings. VOICES results also have value in academic research and have been used in numerous studies, for example, identifying factors influencing quality of care and the impact of pain management on experience of care.
There is also wide public interest in VOICES results, which help to inform differences in quality of care between settings, health conditions and stage of life and can inform lifestyle choices on preferences for care and place of death. Survey respondents in particular have an interest in the results. The full range of uses for official statistics can be seen in The Use Made of Official Statistics (2010).
We welcome feedback from users on the content, format and relevance of this release. Data users can post or email feedback to the address in the background notes section.
Nôl i'r tabl cynnwys