Cynnwys
- Key points
- Introduction
- Public service healthcare output
- Public service healthcare quantity
- Public service healthcare quantity by component
- Contributions to public service healthcare quantity growth
- Quality adjustment of public service healthcare output
- Public service healthcare inputs
- Public service healthcare inputs growth
- Public service healthcare inputs by component
- Contributions to public service healthcare inputs growth
- Policy context
- Revisions
- Triangulation
- Supporting information
- References
- Background notes
- Methodoleg
1. Key points
Public service healthcare has experienced its third consecutive year of productivity growth since 2010. The last period prior to this to experience consecutive years of productivity growth was 2003 to 2006
In 2011, public service healthcare productivity increased by 3.5% - the largest increase since the series began in 1995. Growth in productivity was still positive, but fell back to 0.9% in 2012, due to a decrease in output growth to 2.8% and an increase in input growth to 1.8%
The last two years of positive productivity growth have increased the annual average growth rate for public service healthcare productivity from 0.5% per annum between 1995 and 2010, to 0.8% per annum between 1995 and 2012
The main component of public service healthcare output growth continues to be hospital and community health service activity, while the main component for inputs growth continues to be goods and services rather than labour volumes
There was a smaller than average, but still positive, contribution to public service healthcare output growth from the quality-adjustment factor in 2012
Figure 1: Public service healthcare productivity growth rates, 1996-2012
UK
Source: Office for National Statistics
Download this chart Figure 1: Public service healthcare productivity growth rates, 1996-2012
Image .csv .xls2. Introduction
Public service healthcare productivity is estimated by dividing the total amount of healthcare output by the total amount of input used. Healthcare output is also adjusted for quality (Figure 2). Figures are expressed as indices or growth rates each year, with the starting point of the series in 1995 as the reference year (1995=100). Output and inputs data are estimated at a UK level and are published in calendar years to be consistent with UK National Accounts.
A paper containing details of the data sources and methodology for compiling these statistics is available at ONS (2013a).
Figure 2: Estimating public service healthcare productivity
Source: Office for National Statistics
Download this image Figure 2: Estimating public service healthcare productivity
.png (6.5 kB)This release contains new data for 2011 and 2012 which has enabled a more robust process for estimating healthcare output during the transition of source datasets affected by the Health and Social Care Act 2012.
There have been minor revisions to estimates of output, inputs and productivity between 1995 and 2010 compared to previously published statistics (ONS 2012b) for most years. These are due to changed source data and improved estimates for some unit cost and input deflators.
Reference table available:
Nôl i'r tabl cynnwys3. Public service healthcare output
Public Service healthcare output consists of an estimate of volume (or quantity), which is then adjusted for quality. The quantity of delivered healthcare services is a cost-weighted activity index. Healthcare output consists of the quantity of healthcare adjusted for changes in the quality of delivered services. The reasons for quality-adjusting public service output follow from recommendations made in the Atkinson Review (2005).
Data used to estimate healthcare quantity
The quantity of healthcare is estimated using data on a range of healthcare services provided within the following sectors:
Hospital and Community Health Services (HCHS). This includes hospital inpatient, day case and outpatient episodes. These procedures are distinguished by Health Resource Group (HRG) and up to 2010-11 included some recorded activity provided by non-NHS providers
Family Health Services (FHS). This includes GP and practice nurse consultations, publicly funded dental treatment and sight tests
GP prescribing. This includes all drugs prescribed by General Practitioners
Non-NHS provision. This is the indirectly measured component which uses an inputs=output approach to estimation
Data on HCHS and GP prescribing are provided by England, Wales, Scotland and Northern Ireland health administrations. Wales does not provide FHS data, and at present, no data is available from Northern Ireland on non-NHS provision. Country specific data on quantity is aggregated according to Public Expenditure Statistical Analysis (PESA) weights for current price healthcare spending (HM Treasury, 2014 and previous years).
The collection of datasets for England has been significantly altered, particularly for measuring HCHS activity due to the abolition of the Primary Care Trusts (PCTs) in the Health and Social Care Act 2012. In addition, there was change in the classification of Mental Health and Cystic Fibrosis within the Healthcare Resource Group (HRG) codes, which presented problems in matching like-for-like data series between datasets collected for England in 2010-11, 2011-12 and 2012-13. The Background notes describe the issues and the way in which the output has been calculated in this release in more detail.
Public service healthcare expenditure shares by component
Figure 3 shows the expenditure shares for each component of output for the UK. Hospital and Community Health Services (HCHS) dominate expenditure accounting for almost two-thirds of total expenditure, followed by Family Health Services (FHS) with 17% of total expenditure. GP prescribing costs and expenditure on services provided by non-NHS provision account for the remaining 21% of expenditure1. HCHS and FHS services have been dominant expenditure shares throughout the period, while the share from GP prescribing has fallen as non-NHS provision has increased. Non-NHS provision has increased its expenditure share from around 4% in 1994-95 to over 10% in 2011-12.
Figure 3: Public service healthcare expenditure shares, by output component, 2011-12
UK
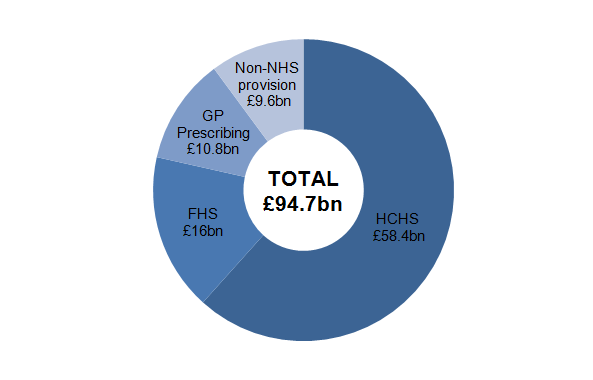
Source: Office for National Statistics
Notes:
- Total may not sum due to rounding
- HCHS = Hospital and Community Health Services
- FHS = Family Health Services
Download this image Figure 3: Public service healthcare expenditure shares, by output component, 2011-12
.png (16.1 kB)Reference table available:
Notes for Public service healthcare output
1.Total spending derived by multiplying measured activity and unit costs by healthcare component plus non-NHS provision covers around 80% of overall Government consumption expenditure on healthcare as reported in UK National Accounts. For the unmeasured elements, which include policy work, prevention, regulation, Arms Length health organisations and administration, there is an implicit assumption that their output moves at the same rate as measured activities.
Nôl i'r tabl cynnwys4. Public service healthcare quantity
Figure 4 shows that healthcare quantity in the UK has been growing continuously for all years of the series. Over the last eighteen years, services have been growing at an average rate of 4.4% per year, but for the most recent four years from 2009-10 to 2012-13 the average growth rate is 2.7%. In 2009-10, quantity growth was 0.6 percentage points below the longer-term average, while in 2010-11, 2011-12 and 2012-13, growth in activity was between 1.5 and 2.0 percentage points lower than average. This is likely to be a reflection of the lower nominal increases in healthcare spending recorded during this period, compared to previous expenditure growth.
In the period before 2009-10, quantity growth averaged 4.8% per year, including 1996-97 which was an exceptionally low volume growth year. With the exception of that one year, growth ranged from 3.6% in 1999-00 to a high of 7.8% in 2003-04.
Figure 4: Public service healthcare quantity growth, 1995-96 to 2012-13
UK
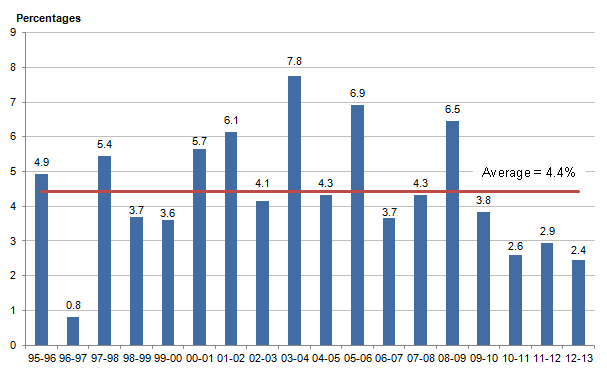
Source: Office for National Statistics
Download this image Figure 4: Public service healthcare quantity growth, 1995-96 to 2012-13
.png (13.7 kB)5. Public service healthcare quantity by component
Figure 5 shows the average growth rates of each of the components of healthcare quantity between 1994-95 and 2012-13. These should be seen within the context of a generally increasing population over the same time period.
Figure 5: Annual average growth rates, by component of public sevice healthcare quantity, 1994-95 to 2012-13
Source: Office for National Statistics
Notes:
- HCHS = Hospital and Community Health Services
- FHS = Family Health Services
Download this chart Figure 5: Annual average growth rates, by component of public sevice healthcare quantity, 1994-95 to 2012-13
Image .csv .xlsHCHS: output has grown by an average of 3.3% per year over the period but with lower growth rates of around 2% per year seen since 2009-10.
FHS: Family Health Services, mostly comprising GP visits and consultations, have grown the slowest at 2.2% per year on average since 1994-95. Growth in FHS has remained at around 2% per year since 2009-10.
GP Prescribing: The volume of GP-prescribed drugs has grown by 7.4% per year on average over the whole series, but lower growth rates of around 3-4% per year have been seen since 2009-10
Non-NHS provision: The largest growth of 13.3% per year (from a low base) is in the volume of services funded by Government but which are provided by non-NHS organisations. This includes:
a range of clinical services sub-contracted by Trusts to the private and independent sector
services commissioned directly by PCTs (now Clinical Care Groups in England) from the private sector
services provided by local government but paid for by the NHS particularly for Continuing Care packages for older people being treated in the community; and
services provided by other charities and non-NHS organisations, again particularly for older people’s care and those with learning difficulties and mental health needs.
Growth in non-NHS provision remains relatively high at around 7% per year since 2009-10.
Nôl i'r tabl cynnwys6. Contributions to public service healthcare quantity growth
The contributions to growth1 in healthcare quantity since 1994-95 are given in Figure 6. This shows that movements in HCHS services are the dominant contribution to healthcare quantity growth, particularly for the peaks in 2005-06 and 2008-09.
Figure 6: Contributions to growth of public service healthcare quantity, 1995-96 to 2012-13
UK
Source: Office for National Statistics
Notes:
- HCHS = Hospital and Community Health Services
- FHS = Family Health Services
Download this chart Figure 6: Contributions to growth of public service healthcare quantity, 1995-96 to 2012-13
Image .csv .xlsAveraging the contributions to growth over the whole time period since 1994-95, of average growth of 4.4% per year, HCHS contributes 2.0 percentage points, GP prescribing 1.2 percentage points, non-NHS provision 0.8 percentage points and FHS 0.4 percentage points.
GP Prescribing: The contribution from GP-prescribed drugs has shown a strong downward trend since 2000-01, declining from a peak of 2.9 percentage points in 2000-01, to contributing just 0.4 percentage points of total healthcare quantity growth in 2012-13. This is similar now to the contribution to growth from the rest of Family Health Services and services provided by non-NHS bodies.
Over the last ten years increases to the volume of drugs prescribed to treat central nervous systems, cardiovascular systems and endocrine systems have contributed over half of the growth of GP prescribed drugs. The most noticeable contributions come from lipid-regulating drugs (including statins), corticosteriods (for the treatment of asthma), and drugs used in diabetes.
While the volume of items GPs prescribe continues to grow, their expenditure weight has been steadily falling over time. This is partly driven by reduced prices for the drugs themselves as administrations have negotiated discounts to expensive drugs, and the increased use of generics (non-branded equivalent) drugs. Nuffield Trust (2014) report that the real Net Ingredient Cost per item prescribed in each country of the UK has fallen by between 25-35% between 2006-07 and 2012-13.
Notes for Contributions to public service healthcare quantity growth
- Contributions to Growth are the growth in volumes of each component of healthcare service, multiplied by (or weighted by) its expenditure share
7. Quality adjustment of public service healthcare output
In line with the recommendations of the Atkinson Review (2005) a quality-adjustment factor is applied to the estimate of healthcare quantity.
ONS (2013a) explains the methodology for the current health quality adjustment in more detail.
The adjustment reflects two measures of quality:
The extent to which the service succeeds in delivering its intended outcomes - there is a measure for HCHS services that reflects short-term survival rates, health gain following treatment in hospital and changes in waiting times. Outcomes from primary care are measured by the percentage of certain groups of patients meeting target ranges for cholesterol levels and blood pressure
The extent to which the service is responsive to users’ needs - the National Patient Survey results are used to gain a measure of patient experience of hospital inpatient services, mental health services, primary care, outpatient and accident and emergency services
Impact of quality-adjustment on public service healthcare quantity
Figure 7 shows the impact of applying the quality-adjustment factor to estimates of healthcare quantity. Over the period from 2002, the quality adjustment adds 0.5 percentage points per year on average to output growth estimates (rounding to 1 decimal place).
The quality adjustment (of 0.01 percentage points) in 2012-13 was the smallest positive adjustment since the series began.
Figure 7: Public service healthcare quantity and quality growth rates, 1995-96 to 2012-13
UK
Source: Office for National Statistics
Download this chart Figure 7: Public service healthcare quantity and quality growth rates, 1995-96 to 2012-13
Image .csv .xlsComponents of public service healthcare quality
Figure 8 shows the contribution to the quality adjustment factor from HCHS and GP services. Survival, health gain and waiting times for HCHS services have provided the greatest contribution to the quality-adjustment factor since 2003-04. Primary care improvements provided a positive contribution to quality-adjustment between 2003-04 and 2006-07, as patients in particular groups were given appropriate treatments, but has tailed off as targets for treatment have approached 100%.
In 2012-13, the increase in quality from GP consultations was largely offset by a reduction in the quality of service from HCHS (as measured by the quality adjustment factor). This is only the second time since the series began in 2003-04 that the quality-adjustment from HCHS fell. This was partly the result of increases to some patient waiting times.
Figure 8: Contribution to growth of the public service healthcare quality adjustment factor, 2003-04 to 2012-13
UK
Source: Office for National Statistics
Notes:
- HCHS = Hospital and Community Health Services
- FHS = Family Health Services
Download this chart Figure 8: Contribution to growth of the public service healthcare quality adjustment factor, 2003-04 to 2012-13
Image .csv .xlsThe output series are collected, largely, on a financial-year basis. To produce a final public service healthcare output series on a calendar-year basis, we apply a splining tool to the quality-adjusted output data which fits equations to the financial year data allowing conversion to calendar years. This approach is commonly used across the Office for National Statistics.
Figure 9 shows the volume of public service healthcare output growth in calendar years using this technique.
Figure 9: Public service healthcare volume growth, 1996-2012
UK
Source: Office for National Statistics
Download this chart Figure 9: Public service healthcare volume growth, 1996-2012
Image .csv .xls8. Public service healthcare inputs
Inputs to publicly-funded healthcare are broken down into three components:
labour input, such as hospital consultants, registrars, nurses, technical staff, ambulance staff and support, General Medical Practitioners (GPs) and practice staff
goods and services input, such as pharmaceutical services, dental and ophthalmic services, and intermediate consumption by hospitals and GP practices. This component also includes GP prescribed drugs and services provided by non-NHS organisations
capital consumption – this is a measure, in volume terms, of the amount of capital stock used each year and is made up of depreciation and other capital charges
Data for estimating healthcare inputs is drawn from a mixture of final consumption expenditure from National Accounts and data from the Health Administrations in England, Wales, Scotland and Northern Ireland. A paper giving further information about the sources, methods and geographic coverage used to calculate the statistics in this release is available (ONS 2013a).
Expenditure shares of public service healthcare inputs
Figure 10 shows that labour expenditure accounts for 51% of total public service healthcare expenditure (£60.9bn) compared to 47% for goods and services expenditure (£55.6 billion) in 2012. Capital consumption accounts for the remaining 2% of the total £118.6 billion.
Figure 10: Public service healthcare inputs expenditure shares, by component, 2012
UK
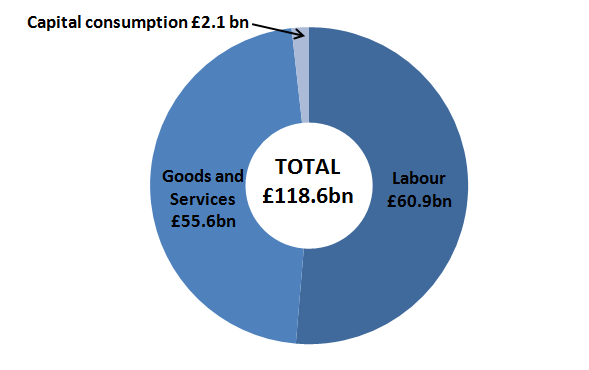
Source: Office for National Statistics
Notes:
- Totals may not sum due to rounding.
Download this image Figure 10: Public service healthcare inputs expenditure shares, by component, 2012
.png (16.3 kB)Reference Table available:
Nôl i'r tabl cynnwys9. Public service healthcare inputs growth
Annual growth in the volume of publicly-funded healthcare inputs for the UK is shown in Figure 11. There have been positive annual growth rates over the entire period, apart from in 2011, when the volume of inputs growth fell to zero. The average growth in public service healthcare inputs over the whole series is 4.0% per year.
Between 2000 and 2010, inputs growth averaged 4.9% per year, but since 2010, inputs growth rates have fallen to 0.9% per year. This slow-down has been driven by a fall in the growth rate for goods and services procurement, from an average of over 7% per year between 1995 and 2010, to 2.8% in the two years since 2010. Labour inputs have also contributed to the slow-down as they have been broadly flat since 2010, compared to 2.6% per year average growth between 1995 and 2010.
Figure 11: Public service healthcare inputs volume growth, 1996-2012
UK
Source: Office for National Statistics
Notes:
- Mean is geometric
10. Public service healthcare inputs by component
Figure 12 shows the average annual growth rates of each of the components of healthcare inputs between 1996 and 2012.
Reference table available:
Table 6: Public service healthcare input indices by component, UK 1995-2012 (28 Kb Excel sheet)
Figure 12: Annual average growth rate for public service healthcare inputs, by component, 1996-2012
UK
Source: Office for National Statistics
Download this chart Figure 12: Annual average growth rate for public service healthcare inputs, by component, 1996-2012
Image .csv .xlsGoods and services: goods and services inputs have grown the fastest at an average of 6.8% per year. This includes volumes of GP prescribed drugs, costs of contracted-out staff working in hospitals and non-NHS provision.
Capital consumption: capital consumption inputs have grown the slowest at 0.5% per year.
Labour: Labour inputs have grown by 2.2% per year over the time series. In 2011, labour inputs across the UK fell for the first time by 1%, then grew 0.2% in 2012.
There were 1,678,383 people employed by the NHS, if you combine the National Health Service1 employees of the four health administrations of the UK in 2012-13. This is more than 5.5% of the employed UK population or the equivalent of 1 in 18 of the workforce.
The largest proportion of the NHS workforce (approximately 30%) is employed as nursing, midwifery and health visiting staff. Approximately a quarter of staff are employed as health care assistants and support workers, and administration and estates staff account for around 23%.
Nearly 176,000 people (one tenth of the NHS) are employed as medical and dental staff in the combined service. This group consists of consultants, registrars, general practitioners (GPs), doctors in training, and other medical and dental staff.
Figure 13 shows data for England only for staff working in the Hospital and Community Health sector and General Practioners from 2006-07 to 2012-13.
Figure 13: Annual percentage change in NHS Hospital and Community Health Services and GP staff, 2006-07 to 2012-13
England
Source: Health and Social Care Information Centre (HSCIC)
Download this chart Figure 13: Annual percentage change in NHS Hospital and Community Health Services and GP staff, 2006-07 to 2012-13
Image .csv .xlsWithin these overall totals, with the exception of 2010-11 (when there was no change from the previous year), the number of professionally qualified clinical staff2 has risen every year since 2006-07. In contrast, the number of NHS infrastructure support and clinical support staff have fallen by nearly 5% between 2010-11 and 2012-13.
Notes for public service healthcare inputs by component
The National Health Service consists of the four publicly funded health care systems in the UK - NHS England, NHS Scotland, NHS Wales / GIG Cymru, and Health and Social Care in Northern Ireland
Professionally qualified clinical staff include qualified nursing staff; qualified scientific, therapeutic and technical staff; HCHS medical and dental staff (consultants, registrars, doctors in training, and other medical and dental staff); GPs; and qualified ambulance staff
11. Contributions to public service healthcare inputs growth
Contributions to public service healthcare inputs growth
Figure 14 shows that with the exception of 2004, goods and services volumes contributed more than increases in labour to the growth in overall healthcare inputs.
Figure 14: Contributions to growth, by public service healthcare inputs component, 1996-2012
UK
Source: Office for National Statistics
Download this chart Figure 14: Contributions to growth, by public service healthcare inputs component, 1996-2012
Image .csv .xlsThe contribution to growth from the labour component of inputs was strongest between 2002 and 2004 at around 3 percentage points. This coincides with the implementation of the NHS Plan, the introduction of Agenda for Change reforms and an expansion in recruitment within the NHS.
Capital consumption input remains broadly flat throughout the series, and only contributes around +/– 0.5 percentage points to overall inputs growth for most years. From 2009, both labour and goods and services showed a steep decline in their contribution to growth of overall inputs. Labour volumes actually shrank in 2011 which, along with a small fall in capital inputs, were offset by a small growth in goods and services, leading to zero growth in overall inputs for 2011. This is the only year in the series that the volume of inputs for the UK healthcare system did not grow at all.
There was a small recovery in inputs growth to 1.8% in 2012, driven by some growth in goods and services and labour inputs.
Nôl i'r tabl cynnwys12. Policy context
The pattern of inputs volume growth, and in particular, the much slower growth rates between 2009 and 2012 compared to previous years, can be seen as reflecting the achievement of the Nicholson efficiency challenge1 in England, and the much lower budget increases experienced in the health service across the UK under Spending Review 2010.
Table 1 shows that the annual average growth rate of current health spending in the UK between 2010-11 and 2013-14 was 3.1% (HM Treasury 2014). This compares with an average growth rate of healthcare current expenditure of 6.3% per year between 2006-07 and 2010-11 (HM Treasury 2011).
The spending pattern across the UK since 2010-11 is broadly in line with the 2.7% growth in the resource Department Expenditure Limit (DEL) settlement (including depreciation) proposed in 2010 for the NHS in England.
The difference between cash expenditure growth rates and volume of inputs growth rates is dependent on the growth of prices and wages in the sector. The Health Service Cost Index, published by the Personal Social Services Research Unit (PSSRU, 2014) shows a slow-down in pay and prices from 2010-11 to 2012-13 to an average of 2.2%, down from an average of 3.3% per year between 2002-03 and 2010-11. This means that cash increases of around 3% translate to real terms increases of up to around 1%. This compares to the higher real terms increases of around 4% in the previous five years (6.3% cash growth with 2.6% pay and prices growth).
Table 1: Resource DEL including depreciation, £ billion; PESA Health expenditure by COFOG, 2010-11 to 2014-15
| £ billion | ||||||
| 2010-11 | 2011-12 | 2012-13 | 2013-14 | 2014-15 | Annual average growth rate % 2010-11 to 2013-14 | |
| NHS (Health) Resource DEL (including depreciation) | 99.8 | 102.6 | 105.2 | 108.2 | 111.1 | 2.7% |
| COFOG 71 (Health) – current expenditure | 114.4 | 117 | 119.5 | 125.6 | - | 3.1% |
| Source: HM Treasury, Spending Review, Table A.10 (2010); HM Treasury PESA Statistical Annex (2014) | ||||||
| Notes: | ||||||
| 1. COFOG (Classification of the Function of Government) | ||||||
| 2. Means are geometric | ||||||
Download this table Table 1: Resource DEL including depreciation, £ billion; PESA Health expenditure by COFOG, 2010-11 to 2014-15
.xls (26.1 kB)The Nicholson Challenge required the NHS in England to make £20 billion savings by the end of the Spending Review period (2013). Alongside the Nicholson Challenge, the NHS in England initiated the QIPP programme (Quality, Innovation, Productivity and Prevention) which had the aim of sharing good practice and providing tools for service providers to improve and streamline the provision of services to better meet patients’ needs. Additional funding in Spending Review 2010 was made available to spend via Local Authorities on social care.
These initiatives came at the same time as the Health and Social Care Act 2012 introduced major reform to the local commissioning of services in England through the creation of the new Clinical Commissioning Groups, replacing Primary Care Trusts.
The result of initiatives to make efficiency savings, and a much lower rate of cash increase than had been seen in the past across the NHS, has resulted in the statistics in this release showing historically small or zero volume increases in labour, goods and services and capital consumption for the years 2010, 2011 and 2012.
Notes for policy context
- The Nicholson Efficiency challenge was to deliver the £20 billion savings in England by the end of the Spending Review period (2015)
13. Revisions
Figure 15 shows that revisions to previously published estimates of healthcare productivity growth (ONS 2012) are less than +/- 0.1 percentage points in each year, except in 2010 when the revision is 1.5 percentage points.
Reference table available:
Figure 15: Revisions to productivity growth, 1996-2010 compared to previous article
UK
Source: Office for National Statistics
Download this chart Figure 15: Revisions to productivity growth, 1996-2010 compared to previous article
Image .csv .xlsThe reason for this larger revision in 2010 is because inputs growth was revised downwards by 1.9 percentage points, and output growth revised downward by 0.3 percentage points. This led to an upward revision in productivity growth of 1.5 percentage points (rounding to 0.1 decimal place). In addition to some revised source data, the underlying reason for the large revision to inputs in 2010 was the correction of the index that is constructed by ONS to deflate some components of goods and services inputs. Previously, the index had failed to take proper account of a change in the reference year of the underlying price index.
Output growth has been revised down by 0.3 percentage points in 2010 because of changed estimates of unit costs for some elements of Family Health Services.
Overall, the annual average growth rate for output for the period 1995-2010 has been revised downwards by 0.1 percentage points from 5.0% to 4.9%. Average growth for inputs have been revised downwards by 0.2 percentage points from 4.6% to 4.4% and average productivity growth has been revised upwards by 0.1 percentage point from 0.4% to 0.5%.
Nôl i'r tabl cynnwys14. Triangulation
There is a large literature on healthcare in the UK, with organisations such as the Kings Fund, Nuffield Trust, NAO, Centre for Health Economics (York University), and Institute for Fiscal Studies (IFS) carrying out research on the performance of the NHS, productivity issues and quality measurement.
In this section we briefly highlight some evidence which relates to ONS estimates in this release on:
output growth and demand pressures
productivity measures and indicators
Demand pressures
Demand for healthcare during the period of this release, particularly for hospital care in the UK, continued to rise. Figure 16 provides data from the National Audit Office (NAO, 2013) and shows a 47% rise in hospital emergency admissions over the period 1997-98 to 2012-13.
Figure 16: Hospital emergency admissions, 1997-98 to 2012-13
England
Source: National Audit Office
Download this chart Figure 16: Hospital emergency admissions, 1997-98 to 2012-13
Image .csv .xlsThere are several reasons for this, including an increasing and ageing population in the UK. The same report finds that health sector providers and commentators suggest that more joint working and better integration is needed between primary, secondary, community and social care services to reduce admissions and to manage those who are admitted more effectively (NAO 2013).
Productivity measures and indicators
Centre for Health Economics: Centre for Health Economics (2014) published productivity figures for the NHS in England up to 2011-12. These showed productivity growth in 2011-12 of between 2.1 and 2.4%. The authors report similar low levels of output and input growth as the ONS statistics in this release, and identify some lags between low input growth feeding through to lower output growth the following year.
Hospital productivity: Nuffield Trust (2012) published a report on hospital productivity in England, and reported evidence that financial pressure on hospitals is associated with “crude” productivity improvements. By “crude” productivity the authors mean that no account is taken for quality.
They also note that in the past, productivity improvement in hospitals has been driven by increased output and activity rather than reducing inputs. There have been reductions in length of stay and increases in day case treatments which have been associated with past efficiency gains.
Typically day case treatment delivers outputs that are equivalent in value, but at much lower cost and at a lower level of input. Nuffield Trust also report that quality and efficiency seem to be positively correlated. This may be due to the diffusion of cost-effective technology in hospitals and getting patient care right first time.
Using data for England, Figure 17 shows the rise in in-patient day cases between 1992-93 and 2012-13. The 0-64 age group account for more day cases than the 65 years and over group, but there has been more rapid growth in the number of day cases for this older group. Day cases for the 65 and over age group have increased by over 500% over the last twenty years, compared to 164% in the 0-64 group.

