1. Main findings
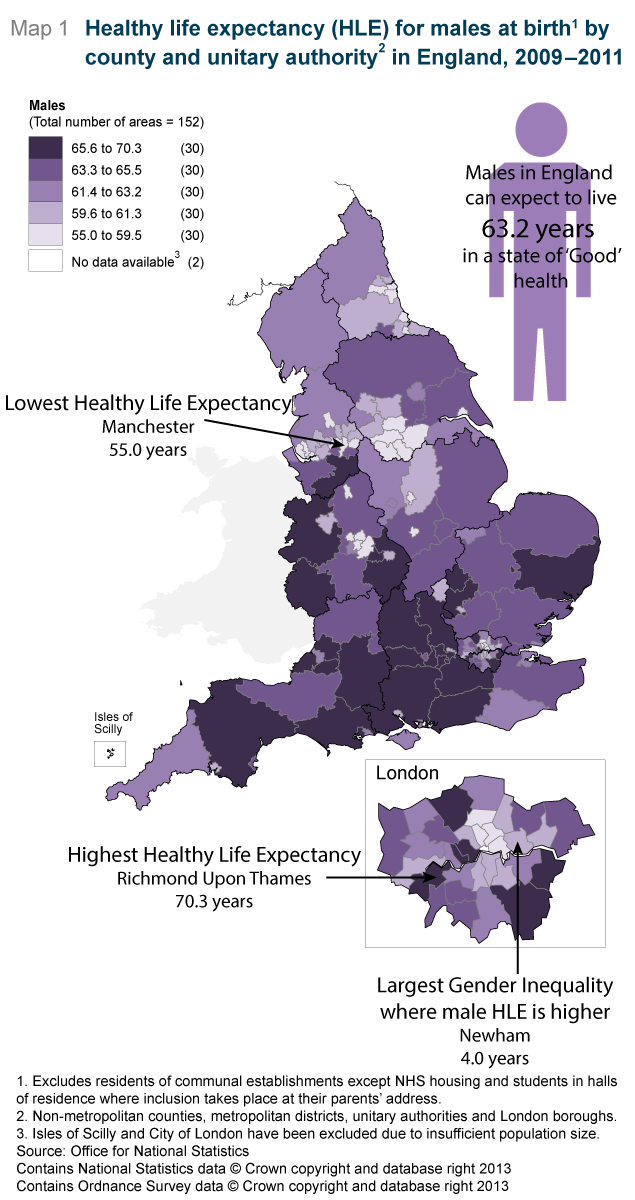
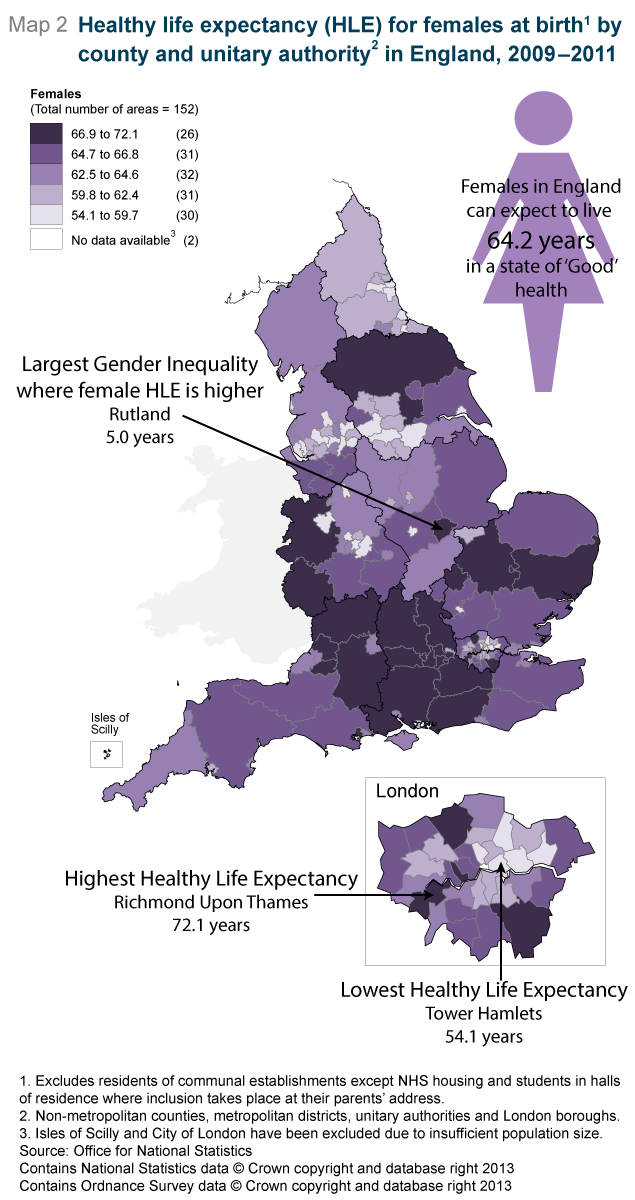
Richmond upon Thames had the highest healthy life expectancy (HLE) for both males (70.3 years) and females (72.1 years).
The lowest HLE was in Manchester for males at 55.0 years and Tower Hamlets for females at 54.1 years.
The inequality in HLE between administrative areas is greater for females than males.
A North South divide in both life expectancy (LE) and HLE exists for both males and females, with HLE in the North East statistically significantly lower than all other regions.
The area inequality in HLE was greater than LE for both genders.
LE was higher for females than males in all areas, but HLE varied.
For males, HLE is significantly higher than the state pension age of 65 in the South East region and in 12 authorities; if females are assessed against the same state pension age, where it will be in 2018, it is higher in the South East, South West and East regions and in 26 authorities.
2. Summary
Health expectancies (HEs) divide predicted lifespan into time spent in given states of health thereby adding a quality of life dimension to estimates of LE. The Office for National Statistics (ONS) routinely publishes two types of health expectancies; Healthy life expectancy (HLE), which estimates lifetime spent in ‘Very good’ or ‘Good’ health based upon self-perceived general health and Disability-free life expectancy (DFLE), which estimates lifetime free from a limiting persistent illness or disability based upon a self-rated functional assessment of health.
HEs are used as a high level outcome to contrast the health status of different populations at specific points in time and to monitor changes in population health over time, giving context to the impacts of policy changes and interventions at both national and local levels. HEs have value across state, private and voluntary sectors, in the assessment of healthy ageing, fitness for work, health improvement monitoring, extensions to the state pension age, pension provision and health and social care need.
This bulletin is the first in the series of estimates of HLE at birth, across English regions and Upper Tier Local Authorities (UTLAs), for males and females. LE figures are presented alongside the HLE figures, these were previously published in the ONS sub-national LE release (ONS, 2013c). The next update of this time series will provide figures for the period 2010-12.
Nôl i'r tabl cynnwys3. Introduction
What are health expectancies?
As life expectancy continues to increase in the UK, it is important to measure what proportion of these additional years of life are being spent in favourable states of health or in poor health and dependency. HEs help us to address this question by adding a dimension of quality of life to estimates of LE. They are estimates of the average number of years a person would live in a given health state if he/she experienced the specified population’s particular age-specific mortality and health status for that time period throughout the rest of his/her life.
The figures represent a snapshot of the mortality and health status of the entire specified area population in each time period. They are not, therefore, the number of years that a person will actually expect to live in the area in a given health state. This is because both mortality and health rates and the exposure risks and treatment effects affecting them, are susceptible to change in the future and because of migration into and out of the area.
Health expectancies are robust indicators of health related well-being and functional status. They are in part estimated through subjective self reports of general health: subjective self reports can be influenced by an individual’s health expectations, which are known to vary across socio-demographic factors such as age, sex, socio-economic position (749 Kb Pdf) (ONS, 2010) and area deprivation (ONS, 2013b).
Self-reported general health and limiting persistent illness are linked (ONS, 2012b, Manor et al., 2001), having some predictive value in subsequent health care need and usage and risk of death. Research evidence has demonstrated people with poor self-rated health (both general health and limiting illness) die sooner than those who report their health more favourably (Mossey and Shapiro, 1982; Idler and Benyamini, 1997; Miilunpalo et al, 1997; DeSalvo et al, 2006; Bopp et al, 2012; Ng et al, 2012).
In terms of morbidity the evidence is more limited; however, studies have shown that self-rated health, measured in terms of both general health and limiting illness, has some predictive value in subsequent health service use in the form of increased physician visits (Miilunpalo et al., 1997) and hospital admission and nursing home placement (Weinberger et al., 1986). Studies have also shown that self-rated health correlates well with retirement due to disability/poor health (Pietilainen et al., 2011; Dwyer and Mitchell, 1999) and poor health outcomes (Lee, 2000).
Survey measurements of general health and limiting persistent illness are used globally to identify health inequality between administrative areas, inform unmet care and health service needs and to target and monitor health care resource allocation amongst population groups (Marmot, 2010). International organisations and networks such as the World Health Organisation (WHO, 2011), Eurostat (Eurostat, 2013) and the Reves network on health expectancy (Reves) use this information to compare morbidity across countries and to monitor trends over time.
This bulletin focuses solely on HLE. These estimates are, in part, subjective and based upon the following survey question.
- ‘How is your health in general; would you say it was…’ – Very good, Good, Fair, Bad or Very bad?
The responses of which are dichotomised to define ‘Good’ general health and ‘Not Good’ general health; ‘Good’ general health is the combination of the very good and good responses and ‘Not Good’ general health the combination of fair, bad and very bad.
HLE is included in both of the two overarching indicators for the Public Health Outcomes Framework (PHOF). The first indicator is increased HLE, taking account of the quality as well as the length of life; the second is to reduce differences in LE and HLE between communities, through greater improvements in more disadvantaged communities. The vision for the indicators is “to improve and protect the nation’s health and wellbeing, and improve the health of the poorest fastest” (page 9, DH, 2012).
The estimates of HLE at birth for England and for UTLAs are calculated using self-reports of general health status collected in the Annual Population Survey (APS), and rely on a method developed by ONS to derive general health state prevalence for persons under 16 years of age (ONS, 2013a) (see methods section). The all England estimate in this bulletin is not comparable with the national health expectancy for the UK and Constituent Countries time series (ONS, 2012b) as the latter output uses a different data source to calculate general health prevalence, namely the General Household Survey (GHS), and the former imputes proxy responses of general health for those aged under 16. For UTLAs wanting to benchmark themselves against a national estimate of HLE, they should do so using the all England estimate in this bulletin and future updates of this series. ONS will cross-validate these sub-national estimates using 2011 Census data with findings due to be published in 2014.
For further information on the implications of differing survey sources, the continuity of the national health expectancies series and the child proxy imputation method please see the update to methodology paper (ONS, 2013a).
HLE focuses on the general health of the population and indicates subjective health-related well-being, including aspects of mental health; however, it does not include a functional assessment of health status, in the form of whether activities are restricted because of any health problems or impairments. Disability-free life expectancy (DFLE) is a measure of the number of years an individual can expect to live free from illnesses or impairments which restrict a person’s ability to carry-out normal day to day activities. The APS includes questions which assess this, so survey respondents can be separated into those who have activity restrictions and those who are free from activity restrictions. The questions used to define these states are recorded below. Only those answering yes to both questions are classified as having a disability and therefore are not disability-free for the purposes of the DFLE measure:
Do you have any health problems or disabilities that you expect will last for more than a year? Yes/No
Do these health problems or disabilities, when taken singly or together, substantially limit your ability to carry out normal day to day activities? If you are receiving medication or treatment, please consider what the situation would be without the medication or treatment? Yes/No
Analysis for this bulletin has been carried out at the UTLA level, which includes counties, London boroughs, unitary authorities and metropolitan districts based on the 2009 re-organisation. Further information about the boundaries can be found on the ONS website. There are 152 UTLAs in England; ONS exclude City of London and the Isles of Scilly from the analysis due to small death and population counts, therefore results are presented here for the 150 remaining UTLAs.
This bulletin comments on a North-South divide. When referred to, the North includes the North East, North West and Yorkshire and the Humber regions and the South includes the South East, South West and East of England regions. London is not included in the South due to its differing characteristics which include its transient population, access to services and limited rural population.
Results are presented with confidence intervals, to aid interpretation. Confidence intervals in this bulletin indicate the uncertainty surrounding HLE estimates and enable more meaningful comparisons between authorities. The confidence interval for each authority enables judgements to be made about whether a given authority has a statistically significant higher or lower HLE estimate compared to another authority, the region within which it resides and England. Differences noted as statistically significant in the text are based on non-overlapping 95% confidence intervals to one decimal place, indicating that there is less than a one in twenty chance of such differences arising as a result of random variation.
Quality information about ONS health expectancies (178 Kb Pdf) is available on the ONS website.
Nôl i'r tabl cynnwys4. Interactive content
Animated map of Healthy Life Expectancy in England [Adobe Flash]
Nôl i'r tabl cynnwys5. Key comparisons
English regions
HLE at birth in England was 63.2 years for males and 64.2 years for females. The pattern across regions shows a prominent North-South divide: HLE in the South East, South West and the East of England was statistically significantly higher than the England average. The West Midlands, North West, North East and Yorkshire and the Humber were significantly lower than the England HLE figure. London and the East Midlands were not statistically significantly different from England (Table 1).
The inequality in HLE between the North and South is wider than that in LE for each gender. HLE was highest in the South East region (65.7 years for males and 67.0 years for females), and lowest in the North East (59.7 years for males and 60.2 years for females). Therefore the inequality in HLE between regions was 6.0 years for males and 6.8 years for females.
The South East, South West and the East have a significantly higher HLE compared with all other English regions for both males and females (Table 1). The North East was unique in that it had significantly lower HLE than all other regions for both males and females, including the North West and Yorkshire and the Humber, suggesting the health profile of the population of the North East is distinct from other parts of England.
HLE for males in the East Midlands, West Midlands, London, Yorkshire and the Humber, North East and North West was significantly below the male state pension age of 65: If we assess females against the same state pension age of 65, where it will be by 2018, the same is true.
The inequality between the North and South can also be seen when looking at the proportion of LE spent in a favourable health state, with males in the South East expected to live 82.1% of their life in ‘Good’ general health compared with 77.1% for their counterparts in the North East region. The same inequality is present among females, where the difference between the two regions is 6.1 percentage points; 80.0% of life expectancy spent in ‘Good’ general health in the South East compared with 73.9% in the North East. For each gender, those living in the southern regions enjoy not only longer life expectancies but also greater proportions of their longer lives in a favourable health state compared with their counterparts living in the North.
Analysing health expectancies in terms of proportion of life spent in a ‘Good’ health state contextualises results, such that we can see whether those who have shorter life and health expectancies also live a shorter proportion of their life in a ‘Good’ health state.
Table 1: Life Expectancy (LE) and Healthy Life Expectancy (HLE) for males and females at birth1 by region2, 2009-11
| England | |||||
| Years, percentage | |||||
| LE | HLE | Lower 95% confidence interval | Upper 95% confidence interval | Proportion of life spent in 'Good' health(%) | |
| Males | |||||
| South East | 80.0 | 65.7 | 65.3 | 66.1 | 82.1 |
| South West | 79.8 | 65.1 | 64.6 | 65.6 | 81.6 |
| East | 79.9 | 64.8 | 64.3 | 65.3 | 81.1 |
| East Midlands | 78.7 | 63.0 | 62.4 | 63.6 | 80.0 |
| London | 79.3 | 63.0 | 62.5 | 63.4 | 79.4 |
| West Midlands | 78.4 | 62.5 | 62.0 | 62.9 | 79.7 |
| North West | 77.4 | 61.0 | 60.7 | 61.4 | 78.9 |
| Yorkshire and The Humber | 78.1 | 61.0 | 60.5 | 61.5 | 78.1 |
| North East | 77.5 | 59.7 | 59.2 | 60.3 | 77.1 |
| England | 78.9 | 63.2 | 63.1 | 63.4 | 80.1 |
| Females | |||||
| South East | 83.8 | 67.0 | 66.6 | 67.5 | 80.0 |
| South West | 83.7 | 66.3 | 65.8 | 66.9 | 79.2 |
| East | 83.6 | 66.2 | 65.6 | 66.7 | 79.2 |
| London | 83.6 | 63.8 | 63.3 | 64.3 | 76.3 |
| East Midlands | 82.8 | 63.3 | 62.7 | 64.0 | 76.5 |
| West Midlands | 82.6 | 62.8 | 62.3 | 63.3 | 76.1 |
| Yorkshire and The Humber | 82.0 | 62.1 | 61.6 | 62.6 | 75.7 |
| North West | 81.5 | 61.7 | 61.3 | 62.1 | 75.7 |
| North East | 81.5 | 60.2 | 59.7 | 60.8 | 73.9 |
| England | 82.9 | 64.2 | 64.0 | 64.3 | 77.4 |
| Source: Office for National Statistics | |||||
| Notes: | |||||
| 1. Excludes residents of communal establishments except NHS housing and students in halls of residence where inclusion takes place at their parents' address. | |||||
| 2. Regions are presented by gender sorted by HLE. | |||||
Download this table Table 1: Life Expectancy (LE) and Healthy Life Expectancy (HLE) for males and females at birth1 by region2, 2009-11
.xls (28.7 kB)7. Gender differences
In every UTLA LE was longer for females than for males. The smallest gender inequality in LE was in Rutland with females expected to live 1.9 years longer than males. The area with the highest gender inequality in LE was Blackpool where females could expect to live an extra 6.2 years.
The gender differences in HLE were less regular in pattern than for LE; while in every UTLA LE for females exceeded that for males, in just over a quarter of UTLAs HLE for males exceeded that for females.
The largest difference in HLE between males and females was seen in Rutland where females can expect to live 5.0 years longer in a state of ‘Good’ general health than males. This was followed by Camden at 4.5 years. In Rutland, it is the high HLE of females rather than the low HLE of males which drives this inequality.
The largest difference between males and females, where males have higher HLE, was in Newham where males can expect to live an additional 4.0 years in ‘Good’ health compared to females. However, it is the lower HLE for females in Newham which drives this gender inequality.
Interesting to note is that although within gender inequality is greater for HLE (HLE: 15.3 years for males and 18.0 years for females) than LE (LE: 8.1 years for males and 6.8 years for females), between gender inequality is greater for LE, at 6.2 years in Blackpool for LE and 5.0 years in Rutland for HLE.
There were only three UTLAs where HLE estimates were the same for males and females, therefore experiencing no gender inequality. These were Leicestershire (65.2 years), Oldham (60.3 years) and Derbyshire (63.0 years).
Nôl i'r tabl cynnwys8. Conclusion
The analysis provided in this bulletin adds a quality of life component to LE estimates. Results for UTLAs, regions and for England are produced to allow comparability across administrative areas for each time point. Producing the three levels of geography allows local areas to compare themselves to the England average, the regional average, with other local areas, and to assess their own improvements over time.
This bulletin has shown a clear North-South divide in HLE, consistent with earlier findings in DFLE for lower tier local authorities. In addition, notable gender differences in LE and HLE are present but the pattern is less uniform in HLE. Female LE is consistently higher than male LE across all the authorities analysed; however, gender differences in estimates of HLE are more varied, with males having a higher HLE than females in just over a quarter of UTLAs.
Inequality in HLE is wider than it is for LE for both males and females. The geographic inequality across UTLAs for females is more than twice as wide for HLE than for LE, 18.0 years and 6.8 years respectively, and for males it is almost twice as wide, 8.1 years for LE and 15.3 years for HLE. Consequently, while geographical inequalities in longevity remain substantial, inequality in HLE is larger. Of the 150 authorities analysed, when assessed with 95% confidence intervals, males on average in 88 authorities have a significantly lower HLE than the state pension age (assessed at 65 for both genders, where it will be by 2018) while for females this is true in 68 authorities.
The English Index of Multiple Deprivation 2010 shows that the northern regions have higher concentrations of LSOAs in the most deprived decile (DCLG, 2011). Previous analyses show that those who live in the most deprived areas, as measured by IMD 2010, have shorter DFLE (ONS, 2013b). This is consistent with the findings in this bulletin which show those in the northern regions and northern authorities predominantly have lower LE and HLE than those in the South.
It is important to track HLE as LE increases, to see whether these years of additional life are spent in states of good health or in poor health and disability; relevant to this are recent changes to state pension age in the UK where people are expected to extend their working lives to take account of improvements in LE. The importance of HLE as a summary measure of population health is reflected in its inclusion in the two high-level outcomes in Public Health England’s Public Health Outcomes Framework.
This bulletin is the first of a future time series of sub-national HLE. This first time period sits wholly within the recent economic recession, and therefore future updates will need to be appraised in the context of period effects related to changes in the economic climate. National and local initiatives designed to narrow the gap between administrative areas, and legislation such as the smoking ban introduced in England in 2007 should also be taken into account. Research has shown the accrual of health benefits, since the implementation of smoke-free legislation in constituent countries of the UK and the Republic of Ireland (Allwright et al., 2005; Pell et al., 2008; Sims et al., 2013).
Nôl i'r tabl cynnwys9. Methods
Calculating healthy life expectancy
This is the first release of sub-national HLE since 2006 (ONS, 2006) which was based on the 2001 Census. These Census estimates were presented at the local authority level for the pre 2009 re-organisation. Insufficient survey sample sizes at a sub-national level have meant that until now, updates to these results have not been possible.
The data used in calculating the prevalence of good general health was obtained from the APS and aggregated over a three year period to achieve sufficiently large sample sizes to enable meaningful statistical comparison.
For this, the first in the series of sub-national HLE estimates using the APS, the period 2009-12 (July 2009 – June 2012) was used for the prevalence of general health as the APS did not begin collecting information on general health until July 2009. Therefore a complete 12 months of data for 2009 is not available. To overcome this shortfall, and to ensure greater accuracy in the estimates and avoid any unwanted seasonal effects, a complete three years of health data from July 2009 – June 2012 was aggregated. The difference between these estimates and those that would have been produced had three years of aggregate data from January 2009 to December 2011 been available was shown to be minimal and would not have altered the principal finding in this bulletin of a large inequality in HLE between UTLAs.
The prevalence of ‘Good’ general health among males and females resident in private households in England was compared across regions and UTLAs, which include unitary authorities, London boroughs and metropolitan districts in England, but excludes the City of London and Isles of Scilly. HLE was then calculated using the Sullivan method which combines prevalence data with mortality and mid-year population estimates (MYPE) over the same period and geographical coverage to calculate estimates of LE and HLE at birth by sex (ONS Life Table Template (192.5 Kb Excel sheet), Jagger, 1999). The MYPEs used to estimate HLE for this bulletin are the revised backdated estimates based on the 2011 census.
The APS provides prevalence information for those over the age of 16. We are able to estimate HLE at birth by directly imputing health prevalence at age 16 -19 for those under 16 (ONS, 2013a).
The age band structure used for calculating HLE is not that outlined in the update to methodology to calculate health expectancies (ONS, 2013a) but the traditional age band structure of <1, 1-4, 5-9, 10-14, 15-19……85+.
Nôl i'r tabl cynnwys10. Interpretation of HLE
HLE at a given age for a specific period and population, such as males and females at birth residing in private households in UTLAs in 2009-11, is an estimate of the average number of years a person would live in a state of ‘Good’ general health if he/she experienced the specified population’s age-specific mortality and health status rates for that time period throughout the rest of his/her life.
The figures reflect the mortality and health status of a population in a given time period residing in that area, rather than those born in an area. It is not therefore the number of years that a person will actually expect to live in the various health states, because both the death rates and health status rates of the specified population are likely to change in the future, because of changes to health risk determinants such as smoking levels in the population, and some of those in the specified population may live elsewhere for part of their lives.
Health expectancies are indicators of health status that take into account differences in the age structures of populations. Results are comparable by age, sex and between specified populations.
Nôl i'r tabl cynnwys