Cynnwys
- Main findings
- Summary
- Introduction
- Survival index for all cancers combined
- Survival index for three cancers combined
- Smoothed maps
- Funnel plots
- Results
- List of figures - smoothed maps
- List of figures - funnel plots
- Notes on methodology
- Users and uses
- Policy context
- Authors
- Acknowledgements
- Additional Information
- References
- Background notes
1. Main findings
The one-year net cancer survival index for England increased from 59.2% for patients diagnosed in 1996 to 68.2% in 2011
Geographic inequalities in the one-year survival index are persistent: a clear North-South gradient existed in 1996, although this was less marked in 2011
The pattern of a gradual increase in the one-year survival index with persistent geographic inequalities is similar for middle-aged (55 – 64 years) and elderly (75 – 99 years) patients
In 2011, the one-year survival index remained on average 20% lower in elderly than in middle-aged patients
Geographic inequalities in the one-year survival index in London are only slightly narrower than those observed for the whole of England
2. Summary
This bulletin presents an index of survival for all cancers combined at one year after diagnosis, for patients who were diagnosed during 1996 – 2011 and followed up to 31 December 2012. The index has been produced for patients living in the territories assigned to each of 211 Clinical Commissioning Groups (CCGs) in England.
Results for additional indices are also presented for patients diagnosed during the same period: (1) a cancer survival index at both one and five years after diagnosis, for all cancers combined, for each of 25 NHS England Area Teams (ATs), and (2) a cancer survival index at both one and five years after diagnosis, for all cancers combined, for England as a whole.
Nôl i'r tabl cynnwys3. Introduction
This report presents the an index of net survival at one year after diagnosis for all cancers combined, for each of the 211 Clinical Commissioning Groups (CCGs) in England. This index is designed to serve as an overall measure of the effectiveness of cancer services at both local and national level. For managerial application, the index needs to reflect the overall outcome (effectiveness) of care for all cancer patients resident in the territory of a given CCG, and to relate to patients diagnosed in a single calendar year.
As a national surveillance tool of strategic value for government policy, the index also needs to provide a succinct national overview of changes in the geographic pattern of short-term survival for all cancers. At both local and national level, trends in the index should support assessment of the impact of earlier diagnosis, a key component of the National Awareness and Early Diagnosis Initiative (Anon. 2008; Richards, 2009a; Richards, 2009b).
Nôl i'r tabl cynnwys4. Survival index for all cancers combined
For each of the 211 Clinical Commissioning Groups in England and for each of the 16 years 1996 – 2011, an index was constructed of one-year net survival (%) for all cancers combined.
In comparing survival between CCGs and over time, it is crucial to take account of differences between CCGs in the profile of cancer patients by age, sex and cancer type. This is because net survival varies with age and sex, and especially between different cancers, and the profile of each of these factors for cancer patients within a given CCG can change over time. Standardisation for all three factors is essential to minimise bias and improve the interpretability of this all-cancers survival index. This approach is encapsulated in the survival index in this bulletin. The approach was developed to produce an index of short-term survival that could be used consistently from year to year for Primary Care Trusts (Office for National Statistics, 2012), which were replaced by CCGs on 1 April 2013.
A cancer survival index has also been constructed on the same basis for each of the 25 NHS Area Teams (ATs) in England over the 16 years 1996 – 2011, at one and five years after diagnosis. The territory of each CCG fits entirely within a given Area Team. A comparable survival index figures has also been constructed for each year for England as a whole.
Nôl i'r tabl cynnwys5. Survival index for three cancers combined
A similar index of survival at one year after diagnosis for three cancers (breast, colorectal and lung) combined has also been constructed for each of the 211 CCGs, for the 25 ATs and for England as a whole, and for each of the 16 years 1996 – 2001.
An index of survival at five years after diagnosis is also presented for each Area Team, and for England as a whole.
Nôl i'r tabl cynnwys6. Smoothed maps
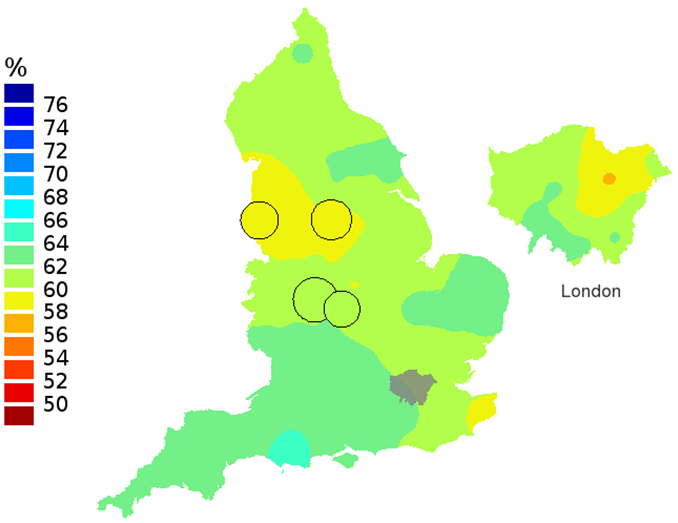
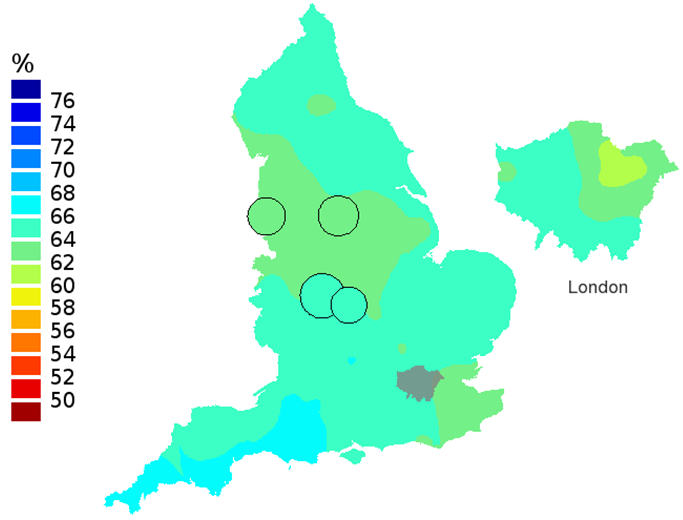
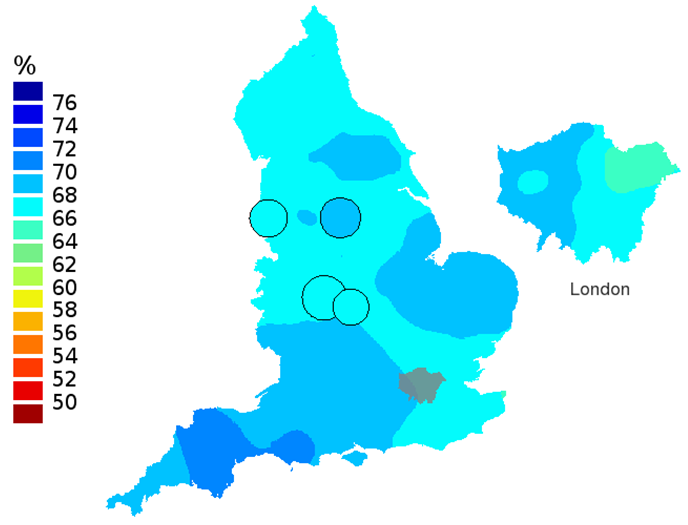
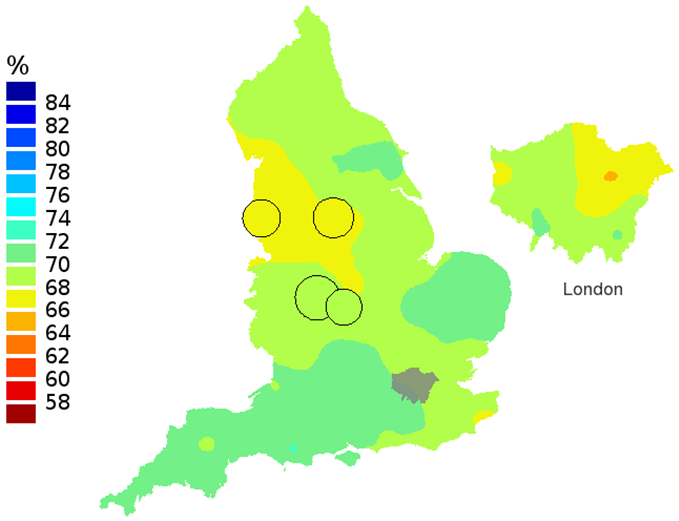
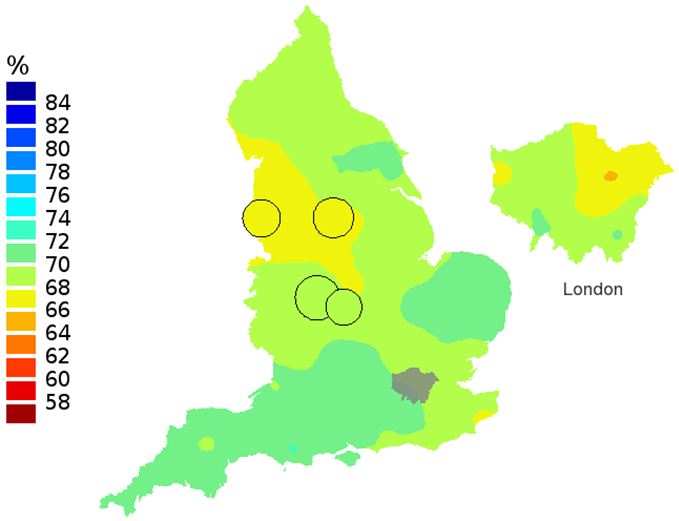
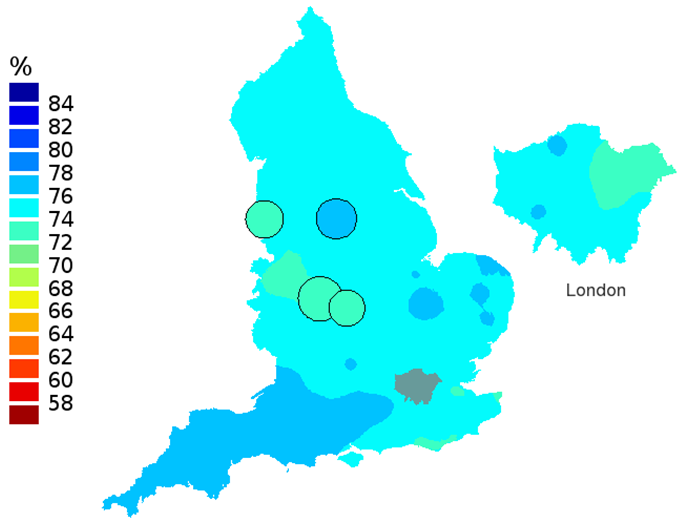
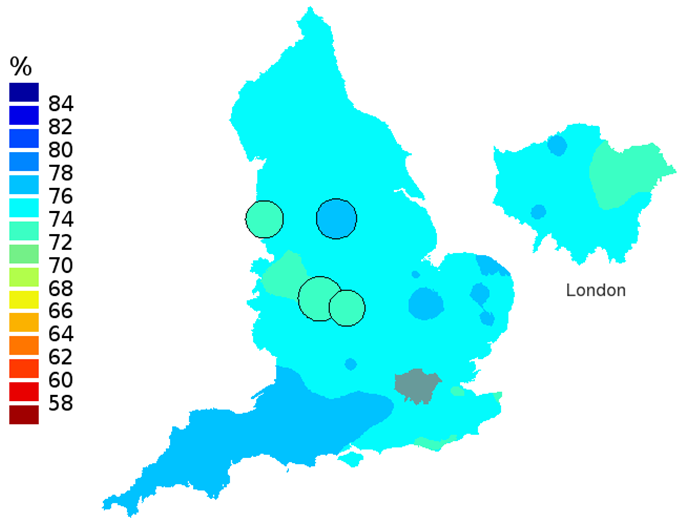
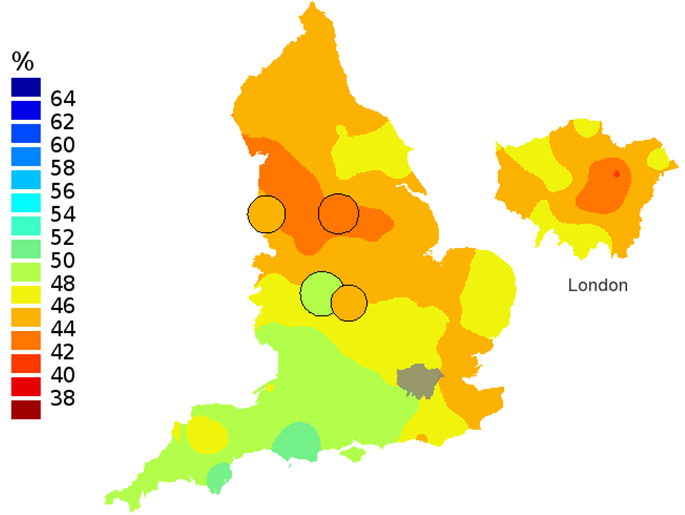
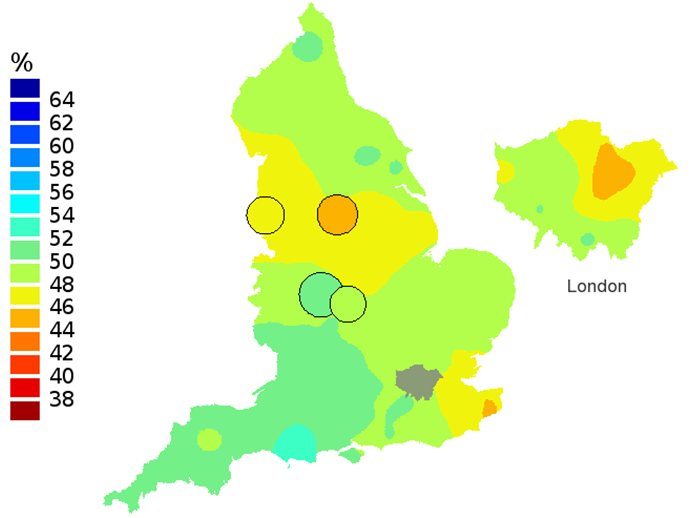
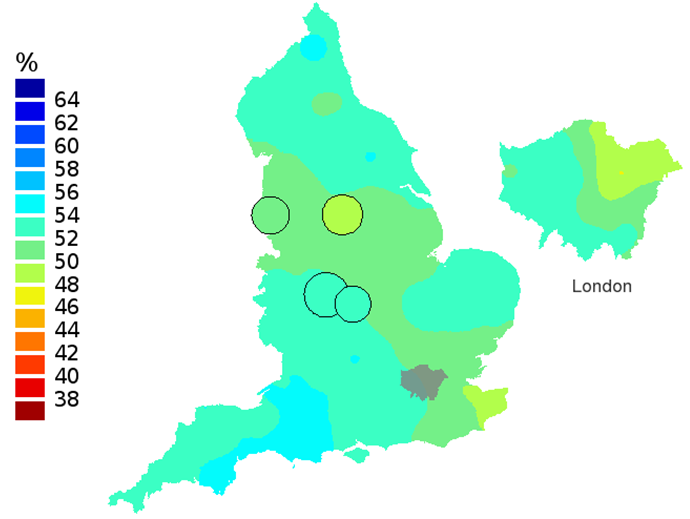
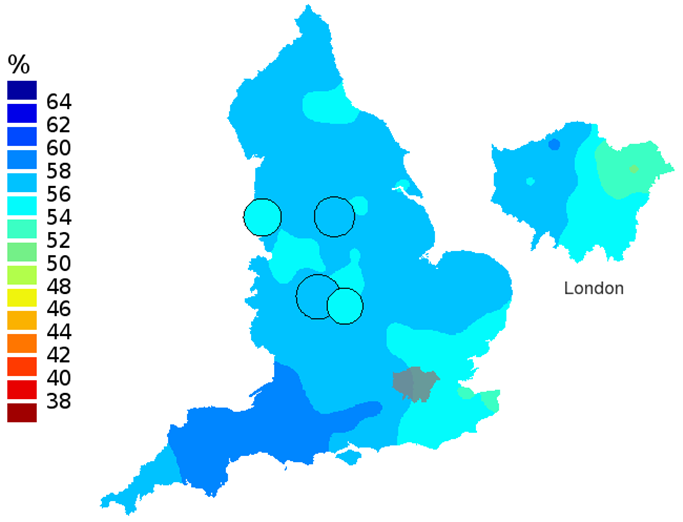
Smoothed maps of the survival index were constructed for each year in the 16-year period 1996–2011 to provide a visual impression of trends in the geographic pattern of one-year survival for all cancers combined across England. Examples are shown for selected years 1996, 2001, 2006 and 2011: one-year survival index for patients aged 15-99 years (Figure 1a – 1d), patients aged 55-64 years (Figure 2a – 2d) and patients aged 75-99 years (Figure 3a – 3d).
In these maps, the CCG boundaries are not shown. The survival index at each point on the map is weighted by all other estimates within a radius of 150km, with weights inversely proportional to their distance. The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process. The purpose of these maps is to provide a ’bird’s-eye’ view of geographic variation in cancer survival across the country, after elimination of random local fluctuations.
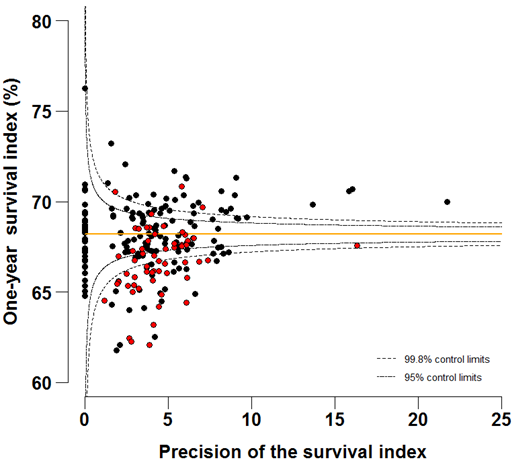
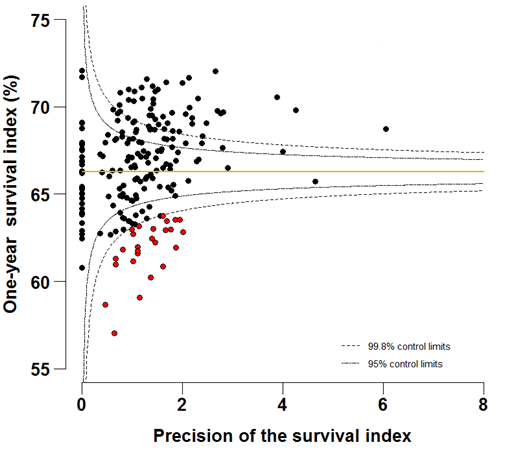
Nôl i'r tabl cynnwys7. Funnel plots
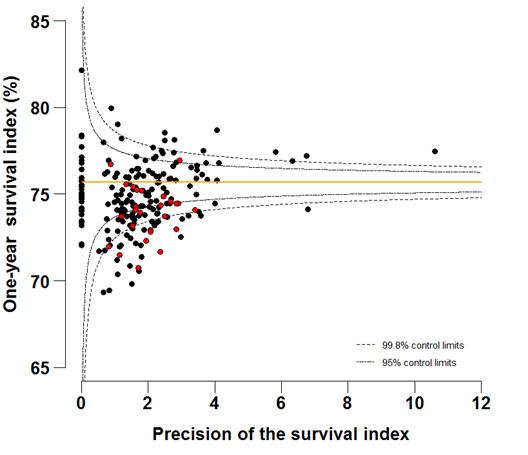
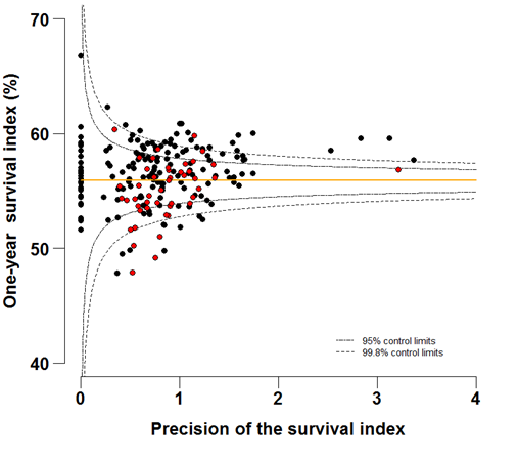
Funnel plots show how much a particular survival index deviates from the overall survival index for that year in England (the horizontal line in each plot), given the statistical precision of the index for each CCG. The precision is the inverse of the variance of the survival index. Funnel plots of the one-year survival index for all cancers combined are presented for all adult patients (aged 15 – 99 years) (Figure 4 – 4b), for patients aged 55 – 64 years (Figure 5a – 5b) and for patients aged 75 – 99 years (Figure 6a – 6b). Each data point represents one CCG.
The two ‘control limits’, in the shape of a funnel around the horizontal line, represent approximately two (95% control limits) and three (99.8% control limits) standard deviations, respectively, above or below the national average. Data points that lie inside the control limits may be considered as within the range of geographical variation that could be expected by chance. Values of the survival index that fell below the control limits for 1996 are marked with a red dot. They represent the CCGs for which the cancer survival index was significantly lower than the national average for patients diagnosed in 1996, after taking account of differences between CCGs in the statistical precision of the index. These CCGs with ‘outlier’ values of the index for 1996 are also marked in red in the funnel plots for the last year of incidence 2011, to provide a visual indication of the extent to which the survival index in those CCGs has improved or remained consistently low over time. It should be noted that these ‘outlier’ values are not just the lowest values that would be obtained from a simple ranked list. Some of the lowest values of the index are still within the range of variation that could be expected by chance (that is, inside the control limits). These are generally for the smallest CCGs, in which the index has lower precision.
Nôl i'r tabl cynnwys8. Results
Table 1 (133.5 Kb Excel sheet) shows the mid-2011 estimates of the resident populations in each CCG (Office for National Statistics, 2013). CCG populations in 2011 covered a more than 14-fold range, from 61,000 to 863,000, with a mean of 252,000.
Table 1 (133.5 Kb Excel sheet) also shows the number of patients included in the analyses for each CCG. Of the 3,262,292 patients who were eligible for analysis, 3.8% were excluded because the cancer was only registered from a death certificate (DCO) and the survival time was therefore unknown. A further 0.3% were excluded because their vital status (whether alive, emigrated, dead or not traced) at 31 December 2012 was unknown, or because of duplicate registration, or an invalid sequence of dates, or because the patient could not be attributed to a CCG of residence at diagnosis. Patients with zero survival time (1.8% of all patients) were included in the analyses, and one day was added to their survival time. Records for multiple primary tumours were excluded (8.2%) to avoid the inclusion of a patient more than once in the estimation of the overall survival index. In all, 2,847,166 patients were included in the analyses.
Estimates of the one-year survival index for all cancers combined are presented for each of the 211 Clinical Commissioning Groups in England, and for each of the years 1996–2011, for all adults (15 – 99 years; Table 2 (630 Kb Excel sheet), for patients aged 55 – 64 years (Table 3 (630 Kb Excel sheet)) and for patients aged 75 – 99 years (Table 4 (630 Kb Excel sheet)).
Estimates of the one-year survival index for three cancers (breast, colorectal and lung) are presented for each of the 211 Clinical Commissioning Groups in England, and for each of the years 1996–2011, for all adults (15 – 99 years; Table 5 (678.5 Kb Excel sheet)), for patients aged 55 – 64 years (Table 6 (678.5 Kb Excel sheet)) and for patients aged 75 – 99 years (Table 7 (678.5 Kb Excel sheet)).
Commentary
For patients diagnosed in 2011, the one-year survival index in England for all cancers combined and for all ages was 68.2% (Table 2 (630 Kb Excel sheet)). This reflects a steady, continuing increase over the last 16 years, from the value of 59.2% for 1996. For patients aged 55 – 64 years at diagnosis (Table 3 (630 Kb Excel sheet)), the index increased from 66.3% in 1996 to 75.7% for patients diagnosed in 2011. The corresponding increase for patients aged 75-99 years (Table 4 (630 Kb Excel sheet)) was from 47.0% in 1996 to 55.9% for patients diagnosed in 2011.
For individual Clinical Commissioning Groups, the trends are generally similar to the overall national pattern, but the range of the survival index between CCGs is wide, from 50.2 to 64.1% in 1996 to 61.8 to 76.2% in 2011 (Figure 4a-4b).
The north-south gradient in one-year survival is a persistent feature of these data, although it has attenuated somewhat between 1996 and 2011 (Figure 1a-1d). Among CCGs in London, the one-year survival index is persistently lower in the north east of the city, although again, the differences are less marked in 2011 than 1996.
Caution is required in interpretation of this overall index of short-term cancer survival for CCGs. The index does not reflect the prospects of one-year survival for any individual cancer patient. It should not be interpreted as if it were the only possible indicator of performance, but in conjunction with other information available to the CCG. It should be seen as a guide, to raise questions about the potential for improvement. The index is designed for use as a tool for public health management of cancer care, both at local and at national level. Not all cancer patients who live (or lived) in the territory assigned to a CCG are (or were) registered with a GP practice included in that CCG.
The index nevertheless provides a convenient, single number that summarises the overall patterns of cancer survival in each CCG, in each calendar year, for men and women, young and old, and for a wide range of cancers with very disparate survival. Survival for most cancers is either stable or rising steadily from year to year (Rachet et al. 2009). This trend is reflected in the values of the index in the tables, but the patterns of cancer occurrence by age, sex and type of cancer can shift quite quickly over time, especially in small areas. The survival index is designed to reflect real progress (or otherwise) by providing a summary measure of cancer survival that adjusts for any such shifts. In short, the index is intended to change only if cancer survival itself actually changes. It is designed for long-term monitoring of progress in overall cancer survival.
Nôl i'r tabl cynnwys9. List of figures - smoothed maps
Figure 1a: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 15-99 years
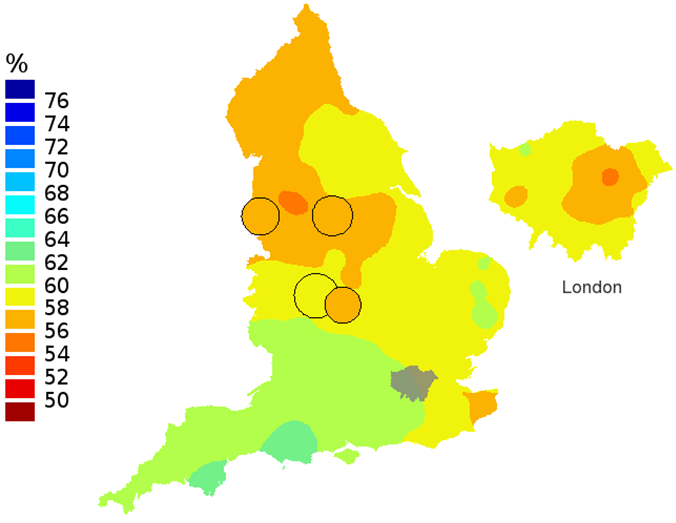
Source: Office for National Statistics, London School of Hygiene and Tropical Medicine
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 1a: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 15-99 years
.png (62.3 kB)
Figure 1b: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2001, patients ages 15-99 years
Source: Office for National Statistics
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 1b: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2001, patients ages 15-99 years
.png (64.0 kB)
Figure 1c: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2006, patients ages 15-99 years
Source: Office for National Statistics
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 1c: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2006, patients ages 15-99 years
.png (61.9 kB)
Figure 1d: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 15-99 years
Source: Office for National Statistics
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 1d: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 15-99 years
.png (55.7 kB)
Figure 2a: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 55-64 years
Source: Office for National Statistics
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 2a: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 55-64 years
.png (63.2 kB)
Figure 2b: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2001, patients ages 55-64 years
Source: Office for National Statistics
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 2b: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2001, patients ages 55-64 years
.png (63.2 kB)
Figure 2c: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2006, patients ages 55-64 years
Source: Office for National Statistics
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 2c: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2006, patients ages 55-64 years
.png (54.6 kB)
Figure 2d: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 55-64 years
Source: Office for National Statistics
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 2d: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 55-64 years
.png (54.6 kB)
Figure 3a: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 75-99 years
Source: Office for National Statistics
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 3a: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 75-99 years
.png (66.3 kB)
Figure 3b: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2001, patients ages 75-99 years
Source: Office for National Statistics
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 3b: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2001, patients ages 75-99 years
.png (65.8 kB)
Figure 3c: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2006, patients ages 75-99 years
Source: Office for National Statistics
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 3c: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2006, patients ages 75-99 years
.png (63.8 kB)
Figure 3d: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 75-99 years
Source: Office for National Statistics
Notes:
- The circles on the maps represent the CCGs with the largest populations, for which survival estimates are statistically stable and are not included in the smoothing process.
Download this image Figure 3d: Smoothed maps of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 75-99 years
.png (57.2 kB)10. List of figures - funnel plots
Figure 4a: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 15-99 years
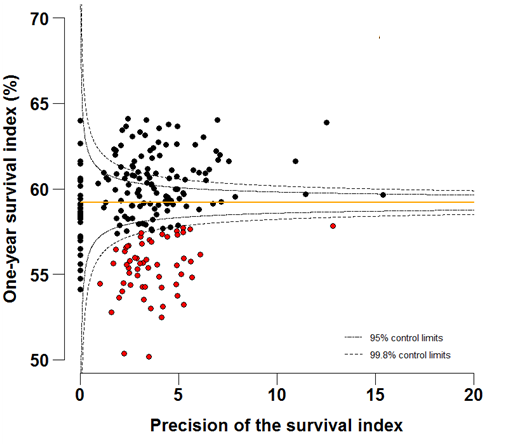
Source: Office for National Statistics, London School of Hygiene and Tropical Medicine
Download this image Figure 4a: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 15-99 years
.png (49.0 kB) .xls (38.9 kB)
Figure 4b: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 15-99 years
Source: Office for National Statistics, London School of Hygiene and Tropical Medicine
Download this image Figure 4b: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 15-99 years
.png (51.0 kB) .xls (48.6 kB)
Figure 5a: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 55-64 years
Source: Office for National Statistics, London School of Hygiene and Tropical Medicine
Download this image Figure 5a: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 55-64 years
.png (48.5 kB) .xls (48.1 kB)
Figure 5b: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 55-64 years
Source: Office for National Statistics, London School of Hygiene and Tropical Medicine
Download this image Figure 5b: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 55-64 years
.png (47.0 kB) .xls (48.1 kB)
Figure 6a: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 75-99 years
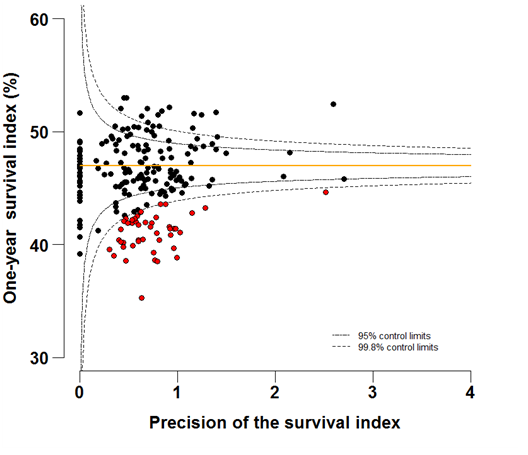
Source: Office for National Statistics, London School of Hygiene and Tropical Medicine
Download this image Figure 6a: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 1996, patients ages 75-99 years
.png (45.5 kB) .xls (48.1 kB)
Figure 6b: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 75-99 years
Source: Office for National Statistics, London School of Hygiene and Tropical Medicine
Download this image Figure 6b: Funnel plots of the one-year survival index (%) for all cancers combined in 211 Clinical Commissioning Groups: England, 2011, patients ages 75-99 years
.png (44.5 kB) .xls (48.1 kB)11. Notes on methodology
The approach adopted to compute the index can be seen as an extension of conventional standardisation by age, to include both sex and the type of cancer.
We have avoided ranking CCGs from the highest to the lowest on the basis of their survival index in any given year, because:
the goal is to provide local information to support long-term improvements in cancer control
if the highest value of the index is (say) 65% and the lowest is 50% (a 15% difference), then with 211 CCGs, a difference of just 1% in the value of the index can mean that the rank of a CCG may change by 10, and by 30 or more in the middle of the range, where differences in the value of the index are very small
the lowest values of the index in a ranked bar-chart for a given year are not necessarily significantly different from what might be expected, because a bar-chart does not take account of the precision of individual estimates
some year-to-year fluctuation of the index must be expected due to chance alone: if a low value for 2011 (say) were the only outlying value for a given CCG in 16 years, and there was no trend for the index in that CCG to fall progressively below the national average, then the low value in 2011 might simply represent random fluctuation
trends also matter. A smaller CCG for which the tables show that the survival index is consistently lower than average should be considering why survival in its area might be low
12. Users and uses
Key users of cancer survival estimates include the Department of Health, academics and researchers, cancer charities, cancer registries, other government organisations, researchers within ONS, the media, and the general public. The Department of Health uses cancer survival figures to brief parliamentary ministers, and as part of the evidence base to inform cancer policy and programmes, for example in drives to improve survival rates. Cancer survival estimates are also used to measure progress against NHS Outcomes Framework indicators. Academics and researchers use the figures to inform their own research. Similarly cancer registries and other government organisations use the figures to carry out individual and collaborative projects to apply subject knowledge to practice. Charities use the data so they can provide reliable and accessible information about cancer to a wide range of groups, including patients and health professionals via health awareness campaigns and cancer information leaflets/web pages. Researchers within ONS use the data to support further research and to publish alongside other National Statistics.
Nôl i'r tabl cynnwys13. Policy context
In ‘Improving Outcomes: A Strategy for Cancer’ (January 2011), the Department of Health stated that although improvements have been made in the quality of cancer services in England, a significant gap remains in survival compared with the European average. Survival estimates for cervical, colorectal and breast cancer are some of the lowest among Member States of the Organisation for Economic Co-operation and Development (OECD). The strategy document sets out how the Department of Health aims to improve outcomes for all cancer patients and improve cancer survival, with the aim of saving an additional 5,000 lives every year by 2014/15.
Outcomes strategies set out how the NHS, public health and social care services will contribute to the ambitions for progress agreed with the Secretary of State in each of the high-level outcomes frameworks. The indicators set for the National Health Service (NHS) Outcomes Framework 2011/12 include one- and five-year net survival from colorectal, breast and lung cancers.
Nôl i'r tabl cynnwys15. Acknowledgements
We are grateful to many persons without whom this work would not have been possible. The continuing efforts of regional cancer registries in England to collect data on all cancer patients to the highest standards of quality and completeness are crucial. The Office for National Statistics collates these data, performs additional quality control and links them to information about each patient’s vital status in the National Cancer Registry.
We gratefully acknowledge Mr Toni Patama and Professor Eero Pukkala at the Finnish Cancer Registry, who kindly provided the software with which the smoothed maps were produced, and who assisted in their production.
Nôl i'r tabl cynnwys