Cynnwys
- Correction
- Main points
- Cancer incidence in England
- The most common cancers registered were breast, prostate, lung, and colorectal cancers
- The 3 most common cancers vary by sex and age group
- Cancer is a disease of ageing
- Cancer incidence varies across England
- What statistics do we calculate?
- Cancer registration data collection in England
- Data quality
- Users and uses of cancer statistics
- Policy context
- References
- Background notes
- Methodoleg
1. Correction
An error was found in the percentage difference in the female cancer incidence rate between the South West of England and London, which was located in the "Cancer incidence varies across England" section of this release. We would like to assure you that this error was minor, and the overall story has not been affected. This was corrected on 10 July 2015 at 4.00pm. We apologise for any inconvenience caused.
Nôl i'r tabl cynnwys2. Main points
In England there were 292,680 invasive malignant cancer diagnoses (excluding non-melanoma skin cancer) registered in 2013. After age-standardisation there were 683.1 cases of cancer registered per 100,000 males, and there were 542.2 cancer cases per 100,000 females. Compared to 10 years ago, the age-standardised cancer incidence rate has risen by 2.8% for males, and 8.3% for females
Breast, prostate, lung, and colorectal cancer accounted for over half of the malignant cancer registrations in England for all ages combined
Broken down by age, leukaemia was the most common cancer in children aged 0 to 14. In teenagers and adults aged 15 to 49, male testicular cancer and female breast cancer were the most common cancers diagnosed. From the age of 50, prostate and breast are the most common cancers for males and females respectively
The cancer incidence rate was 11.5% higher (for all persons) in the North West of England compared with London after taking into account differences in the age structure of their respective populations. When focusing on different cancer sites the regional differences changed. For example, the prostate cancer incidence rate was 30.5% higher in the South East of England compared with the North East
3. Cancer incidence in England
In England, there were 292,680 invasive malignant cancer diagnoses registered in 2013. There were 149,818 new cases of cancer registered for males and 142,862 for females in 2013. The age-standardised cancer incidence rate indicates that there were 683.1 (males) and 542.2 (females) cancer cases per 100,000 people in England in 2013. The age-standardised cancer incidence rate was 26.0% higher for males than females. Compared to 10 years ago, the age-standardised cancer incidence rate has risen by 2.8% for males, and 8.3% for females. In 2004 the rate was 664.8 (males) and 500.7 (females) cases per 100,000 people.
Over 90% of cancer cases were registered in 24 sites in the body (as shown in Figure 1). Breast (female), prostate (male), lung (C33 to C34), or colorectal (otherwise known as bowel cancer; ICD-10 C18 to C20) continue to make up over half of cancer cases registered. These 4 cancers are found to be the most common cancers across the UK1, and worldwide2.
Figure 1: The number of cancer registrations by the 24 major sites, England, 2013
Source: Office for National Statistics
Notes:
- The International Classification of Diseases Tenth Revision (ICD-10) was used to classify cancer sites. Non-melanoma skin cancers (ICD-10 C44) were excluded
- All ages combined
- In England 292,680 new cancer diagnoses were registered in 2013
- The majority (93%) of these cancer registrations are registered in 24 sites of the body
- Just over half (53%) of registrations are breast, prostate, lung and colorectal cancer
Download this chart Figure 1: The number of cancer registrations by the 24 major sites, England, 2013
Image .csv .xlsBy most common we mean the 3 cancers (by sex) with the greatest number of cases registered in 2013. Furthermore, we look at only cancers, which are coded in the International Statistical Classification of Diseases, Tenth Revision (ICD-10) as C00 to C97, excluding C44 (non-melanoma skin cancer), and therefore exclude D00 to D48.
Nôl i'r tabl cynnwys4. The most common cancers registered were breast, prostate, lung, and colorectal cancers
Malignant breast cancer was the most common cancer diagnosed in females (all ages combined), with 44,540 cases registered in 2013. Female breast cancer accounted for 31.2% of total female cancer registrations. The age-standardised incidence rate for breast cancer has increased by 5.5% in 10 years, from 161.0 (2004) to 169.8 (2013) cases per 100,000 females.
Prostate cancer was the most common cancer diagnosed in males (all ages combined) in 2013, with 40,372 cases registered, which accounted for 26.9% of total male cancer registrations. The age-standardised cancer incidence rate for prostate cancer was 185.7 cases per 100,000 males. In comparison to 2004 (174.7 cases per 100,000 males) the age-standardised rate for prostate cancer has increased in the last 10 years by 6.3%.
The second most common cancer for males and females was lung cancer. In 2013, there were 36,653 (19,830 males, and 16,823 females) cases of lung cancer registered in England. Lung cancer accounted for 13.2% (males) and 11.8% (females) of the total cancer registrations. The age-standardised lung cancer incidence rate was 43.6% higher in males than in females; where 92.5 cases per 100,000 males were registered in 2013, and 64.4 cases per 100,000 females. In comparison to 10 years ago (2004) the age-standardised rate for lung cancer has decreased by 9.9% for males and increased by 18.4% for females. The different trends in lung cancer incidence rates for males and females are likely to reflect the change in smoking patterns, where women started smoking more and men less after the Second World War3.
In England, there were 18,839 and 14,926 cases (total: 33,765) of colorectal cancer registered for males and females respectively in 2013. Colorectal cancer accounted for 12.6% (males) and 10.4% (females) of the total cancer registrations. In 2013, there were 86.8 cases per 100,000 males diagnosed with colorectal cancer and 56.2 cases per 100,000 females. The age-standardised colorectal cancer incidence rate was 54.4% higher in males than in females. Over the last 10 years, the age-standardised incidence rate for colorectal cancer has increased for both males and females, however, between 2012 and 2013 there was a drop in the number of cases registered.
There are many risk factors associated with cancer, and there are multiple combinations of risk to consider. Research has indicated that environmental and lifestyle factors such as tobacco smoking, alcohol consumption, obesity, lack of physical exercise, occupational hazard exposures, and diet are linked to cancer4. Genetic, hormonal, and reproductive factors are also related to cancer risk. More information on the risk factors associated with cancer can be found on the National Health Service website5.
Nôl i'r tabl cynnwys5. The 3 most common cancers vary by sex and age group
Prostate, breast, lung, and colorectal cancer are found to be the most common cancers across the UK countries1, and worldwide2. Yet it is interesting to note that the most common cancers vary by sex and age group as Figure 2 and 3 show. For instance:
leukaemia, brain, non-hodgkin’s lymphoma (males), and kidney (females) were the most common cancer registrations in childhood (0 to 14 years old) - these cancers accounted for over half of the 1,359 cancer cases registered in children
for males aged 15 to 49, testicular, skin melanoma, and bowel cancer were the 3 most common cancer registrations - for females the most common cancer registrations were breast, skin melanoma and cervical cancer
from the age of 50, prostate, breast, lung, and colorectal cancer were the most common cancer cases registered
It should be mentioned that the most common cancers vary by the age group used to categorise the data. The age groups we use were chosen to align with the age breakdown in our cancer survival bulletins, which are designed to align with the NHS Outcomes Framework Indicators.
Figure 2: The most common cancers for males by age group, England, 2013

Source: Office for National Statistics
Notes:
- Excluding non-melanoma skin cancer (ICD-10 C44)
Download this image Figure 2: The most common cancers for males by age group, England, 2013
.png (142.0 kB)
Figure 3: The most common cancers for females by age group, England, 2013
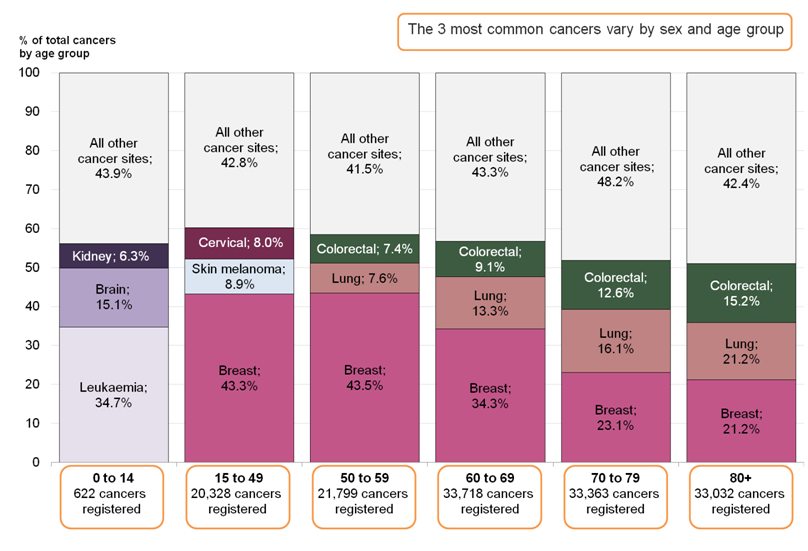
Source: Office for National Statistics
Notes:
- Excluding non-melanoma skin cancer (ICD-10 C44)
Download this image Figure 3: The most common cancers for females by age group, England, 2013
.png (133.3 kB)6. Cancer is a disease of ageing
The majority of cancer cases are registered in the older age groups. Cancer occuring in children, teenagers and young adults (0 to 24) are rare, registrations in this age group accounted for 1.1% of the total cancer registrations. Whereas, cancer registrations for those aged 70 and above accounted for 49.9% of the total registrations. Figure 4 shows the age-specific cancer incidence rate noticeably increasing with age (up until age group 90 and over for females, where it decreases), demonstrating that cancer is mainly a disease of ageing.
The World Health Organisation (WHO) explains that ageing is “a fundamental factor for the development of cancer. The incidence of cancer rises dramatically with age, most likely due to a build up of risks for specific cancers that increase with age”2.
Figure 4: Age-specific cancer incidence rates (per 100,000 people) in 2013, England
Source: Office for National Statistics
Notes:
- Excluding non-melanoma skin cancer (ICD-10 C44)
- Cancer is mainly a disease of the elderly, with the age specific cancer incidence rate increasing with age
Download this chart Figure 4: Age-specific cancer incidence rates (per 100,000 people) in 2013, England
Image .csv .xls7. Cancer incidence varies across England
Map 1: Age-standardised incidence rates by English region, all cancers, all persons, 2013
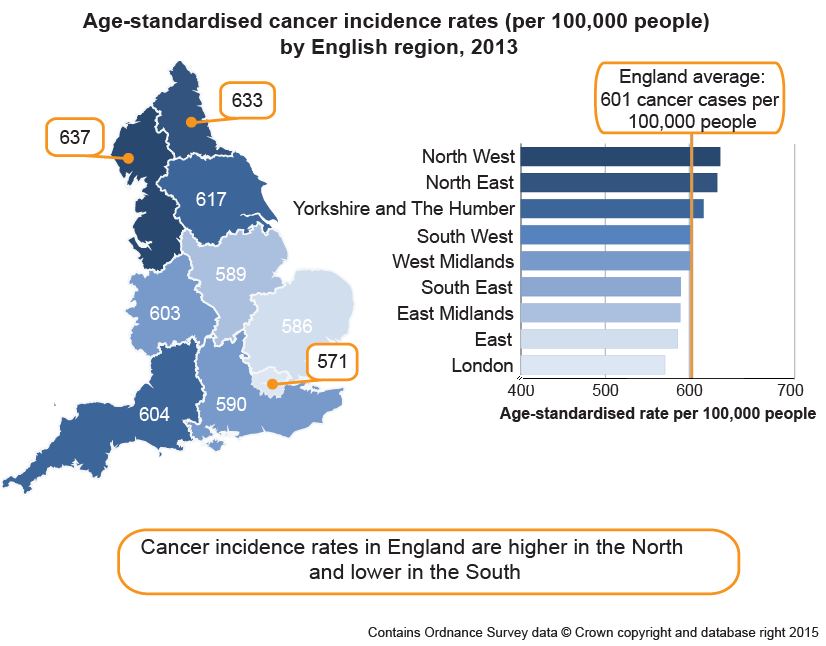
Source: Office for National Statistics
Download this image Map 1: Age-standardised incidence rates by English region, all cancers, all persons, 2013
.png (95.0 kB)- Excluding non-melanoma skin cancer (ICD-10 C44)
Download map data (293 Kb Excel sheet)
The age-standardised cancer incidence rate in 2013 varied across the English regions. For all persons, the rate ranged from 571.0 (London) to 636.6 (North West) per 100,000 people, and the average in England was 601.2 (as shown in Map 1). The age-standardised cancer incidence rate was 11.5% higher in the North West compared to London.
It is important to note that caution should be taken when interpreting regional variations; the differences might be due to a number of influencing factors rather than being a true difference in cancer incidence. One reason might be the variation between regions in deprivation; high levels of deprivation have been associated with higher levels of certain types of cancer6,7. Furthermore, any differences in lifestyle behaviours between regions, for example the regional variance in smoking prevalence8. Specific factors should also be considered like prostate-specific antigen testing a which is not a national screening programme and any regional differences in the availability and uptake of this test could explain regional differences in the age-standardised rate.
When looking at the lowest and highest age-standardised rate the regional variations differ by specific cancers, for example:
the female breast cancer incidence rate was 12.0% higher in the South West of England than in London - in the South West of England there were 178.9 cases per 100,000 females, whereas 159.8 cases per 100,000 females were registered in London
the rate for prostate cancer was 30.5% higher in the South East of England (201.2 cases per 100,000 males) than in the North East (154.2 cases per 100,000 males)
for males, lung cancer rates were 50.8% higher in the North East of England (116.7 cases per 100,000 males) compared to the South East (77.4 cases per 100,000 males), for females in the North East of England (102.2 cases per 100,000 females), the rates for lung cancer were double that of those in the South East (50.5 cases per 100,000 females)
for males, the colorectal cancer incidence rate was 24.6% higher in the North East (97.1 cases per 100,000 males) compared to London (77.9 cases per 100,000 males) - whereas, for females, the colorectal cancer incidence rate was 24.5% higher in the South West (60.9 cases per 100,000 females) compared to London (48.9 cases per 100,000 females)
8. What statistics do we calculate?
Cancer incidence rate: the number of new cancer registrations in a specific population during a particular time period per 100,000 people. Or:
Cancer incidence rate = (total number of cancer registrations/total population) x 100,000
A cancer incidence rate can be calculated by specific age groups, this is referred to as an age-specific cancer incidence rate. We calculate cancer incidence rates for ICD-10 codes C00 to C97 and D00 to D48, all of which can be found in the reference table provided.
Age-standardised cancer incidence rate: a weighted average of the age-specific cancer incidence rates, the weights used are age specific proportions of a standardised population (2013 European Standard Population (ESP)). By standardising cancer incidence rates with the ESP geographical and time comparisons can be made, as the differing age structure of a particular population has been accounted for.
Also included in our reference tables are:
Mortality to incidence ratios: cancer mortality to incidence ratios, are calculated by dividing the number of cancer-related deaths by the number of cancer diagnoses for each given cancer site, sex and region. It must be pointed out that the number of cancer related deaths might include people who were diagnosed before 2013, therefore caution should be made when interpreting these statistics.
Standardised Registration Ratio (SRR): a cancer incidence rate (age and sex specific) is taken as a standard rate; we take England as the standard. The standard rate is then applied to another index population of known age structure (for example, the South West region of England) to calculate how many registrations would have been expected in this index population had they, at each age group, experienced the standard cancer incidence rate (in this example England). The “expected” incidence is then compared to the observed incidence rate in the index population (in this example the South West), with the ratio being multiplied by 100 to give the standardised registration ratio, in which 100 is the value for the standard rate (in this example England). A SRR of 106 would mean the cancer incidence in the index region (in this example the South West) is 6% higher than the standard rate (England). Conversely, an SRR of 94 would mean the cancer incidence was 6% lower.
Nôl i'r tabl cynnwys9. Cancer registration data collection in England
Cancer registrations in England are submitted to us by the National Cancer Registration Service (NCRS) in Public Health England (see Background note 5). The registration of cancer cases is a dynamic process where the data files, both at NCRS and at ONS, are always open and changing. Cancer data files are dynamic in a number of ways:
new cancer cases will be registered: this can include new “late” registrations, where a case is registered after the cancer registry or ONS, or both, have published for a particular year
cancer records can be amended: for example, the site code of a record would be modified if later more accurate information become available
cancer records can be cancelled, although this is unusual
Data are submitted to the NCRS from a range of health care providers and other services (for example, pathology laboratories). As the data come from different sources, the quality and accuracy of the data submitted may vary.
The NCRS carefully collate and validate all the data for each patient, before sending a subset of the data, defined as the cancer registration minimum data set, to the National Cancer Registry at ONS for further validation and processing. The extensive checks run by us include the compatibility of the cancer site and the associated histology, and are closely based on those promoted by the International Agency for Research on Cancer9.
Once all the expected records for any one incidence year have been received and validated we take a snapshot of the data set, which allows us to publish the numbers and rates of all types of cancer by age and sex, and by region of residence. Cancer incidence tables for this release were created in May 2015. It is important to remember that the snapshot of cancer registration data will be different year on year due to the dynamic nature of the data set. Therefore, you will find that the incidence count for 2012 (for example) differs in the current publication compared to the previous publication.
Taking a new snapshot of the dynamic National Cancer Registry database usually results in a difference between what was previously published and what is published from the most current snapshot of data. The balance between ensuring completeness of the data but publishing cancer incidence figures in a timely manner is necessarily a compromise. The gap between what was first published for a registration year and the most recent cancer incidence figures has varied considerably over time, as shown in Figure 5. Over the 42-year period reported, differences between what has been previously published and the current number (refreshed in 2015) of registrations for each year average less than 5%.
Figure 5: Number of cancer registrations previously published in the annual report (MB1 series) and currently on the ONS National Cancer Registry database, England, 1971 to 2012
Notes:
- Figures for 1971 to 1994 have been extracted from the “frozen” historical data set
- The published figures for 1971 to 1978 correspond to all malignancies, not all registrations. From 1979, the numbers refer to all malignant and benign cancer registrations including non-melanoma skin cancer (C44)
- Refreshed figures at May 2015. Previously published figures are taken from the corresponding cancer registration report. For example, figures for 2012 were taken from the report published in June 2014
- The refreshed data in 2015 will generally be higher than what was previously published for a particular registration year. This is because new registrations are constantly being added to the National Cancer Registry data base
Download this chart Figure 5: Number of cancer registrations previously published in the annual report (MB1 series) and currently on the ONS National Cancer Registry database, England, 1971 to 2012
Image .csv .xls10. Data quality
The figures for numbers and rates of "all cancers" in this release refer to all invasive malignant neoplasms (ICD-10 C00 to C97), excluding non-melanoma skin cancer (ICD-10 C44). Although non-melanoma skin cancer (NMSC) is very common the available figures are known to be under-estimates and unreliable for comparison purposes. This is becausethe policies and practices for the recording of NMSC have varied among the cancer registries. Therefore NMSC registrations have been excluded from the figures for ‘all cancers’ in this publication.
Other data quality matters for this year's figures include:
numbers relating to malignant neoplasm of placenta (C58) in London have low reliability due to a potential coding error for a small number of registrations discovered in a late stage of the publication process
the increase in cases of in-situ breast tumours (D05) seen in 2013 is due to a change in coding rules in England; before the change, if an in-situ breast cancer was registered and then, in a close period of time, the patient was diagnosed with an invasive breast cancer in the same breast, the registry concluded this was a progression of the original tumour, and removed the in-situ tumour registration, changing it to an invasive registration - the cancer registry are now recording both cases, unless the second cancer is known to be a progression of the first cancer
since 2008 there has been a large decrease in the registrations of carcinoma in situ of skin (D04) as it is no longer a condition registered
any regional differences in benign, uncertain and unknown neoplasms should be interpreted with caution as there is known historic variation in the way cancer registries recorded these tumours across the country, and they do not receive as much analytical attention and scrutiny as the invasive cancers.
Further details about the cancer registration data can be found in the Cancer Registration Statistics Quality and Methodology Information paper (189.7 Kb Pdf)10.
Nôl i'r tabl cynnwys11. Users and uses of cancer statistics
Main users of cancer registration statistics include:
Department of Health
academics and researchers
cancer charities
cancer registries
other government organisations and our own researchers
the media
general public
The main uses of cancer registration statistics include:
providing an evidence base to inform cancer policy and programmes
informing cancer research
feeding into cancer information leaflets, web pages, campaigns to raise cancer awareness
we use the data to produce National Statistics on cancer incidence and survival
briefing parliamentary ministers
providing answers to parliamentary questions
providing bespoke tables for customers
12. Policy context
Cancer incidence (number of cancer cases registered) data allow policy makers to measure the extent of cancer within the population in England. Cancer incidence data is used alongside cancer prevalence, mortality and survival to allow policy makers to ascertain the burden of cancer in England.
Cancer incidence data directly helps to form policy on the prevention of cancer. It also is important in calculating cancer survival (in conjunction with mortality data) which is then used to drive a number of policy streams within government, and also monitor a number of performance indicators for the English health care system. The indicators set for the NHS Outcomes Framework 2015 to 2016 – focus on measuring health outcomes11 include 1- and 5-year cancer survival indicators for all cancers combined, and for colorectal, breast and lung cancers combined. These survival estimates are calculated from the cancer incidence data.
Nôl i'r tabl cynnwys
