Cynnwys
- Other pages in this release
- Main points
- Socioeconomic inequalities in avoidable mortality
- Socioeconomic inequalities in avoidable mortality by cause
- The Slope Index of Inequality (SII) in avoidable mortality
- Socioeconomic inequalities in avoidable mortality in England data
- Glossary
- Measuring the data
- Strengths and limitations
- Related links
1. Other pages in this release
Socioeconomic inequalities in avoidable mortality in Wales: 2018
Nôl i'r tabl cynnwys2. Main points
The proportion of total deaths in 2018 that were avoidable in England is substantially larger in the most deprived areas compared with the least deprived areas.
Avoidable deaths accounted for nearly two-fifths (39.4%) of all male deaths in the most deprived areas of England compared with less than one-fifth (17.7%) in the least deprived areas in 2018; for females it was 26.2% and 12.2% respectively.
While avoidable mortality rates are sizeably lower than they were in 2001 across all levels of area deprivation, since 2013 the speed of improvement has reduced substantially particularly in the most deprived areas.
The absolute difference in the rate of avoidable death caused by diseases of the circulatory system and injuries, between the most and least deprived areas of England, narrowed between 2001 and 2018; the absolute gap widened for diseases of the respiratory system and alcohol-related and drug-related disorders.
For males and females there were statistically significant decreases in the absolute inequality in avoidable deaths between 2001 and 2018; however, a slowing of improvement is evident in the second decade.
The absolute inequality in the rate of avoidable mortality indicated there were 396.7 additional deaths per 100,000 males living in the most deprived areas of England compared with the least deprived areas and 234.8 additional deaths per 100,000 females living in the most deprived areas compared with the least, in 2018.
3. Socioeconomic inequalities in avoidable mortality
Data in this release have been created using the new international avoidable mortality definition (DOC, 421KB). When discussing avoidable deaths, the following terms are used:
preventable mortality – deaths that can be mainly avoided through effective public health and primary prevention interventions
treatable mortality – deaths that can be mainly avoided through timely and effective healthcare interventions, including secondary prevention and treatment
avoidable mortality – deaths defined as either preventable or treatable
In 2018, the male age-standardised avoidable mortality rate in the most deprived areas of England (decile 1) was 553.3 deaths per 100,000 males, a statistically significant higher rate than the 152.6 deaths per 100,000 males observed in the least deprived areas (decile 10). Similarly, the female age-standardised avoidable mortality rate also showed a statistically significant contrast, amounting to 347.1 deaths per 100,000 females in the most deprived areas compared with 101.5 deaths per 100,000 females in the least deprived areas (Figure 1).
The rate of avoidable death in general reduced as deprivation lessened. Statistically significant reductions were observed between all adjacent deciles along the deprivation scale for each sex apart from deciles 8 and 9. Therefore, males and females living in decile 1 (most deprived areas) had statistically significant higher avoidable mortality rates than the nine other deciles, and males and females living in decile 10 (least deprived areas) had statistically significant lower rates than the nine other deciles. The largest absolute gap was between areas located within deciles 1 and 2 for both sexes, demonstrating avoidable mortality rates were contrasting even between relatively deprived populations.
When comparing males and females in the same deciles, males had statistically significant higher avoidable mortality rates than females. However, males living in deciles 4 and higher had a statistically significant lower rate of avoidable mortality than females living in decile 1.
Figure 1: Males and females living in the most deprived areas had statistically significant higher avoidable mortality rates than those living in the least deprived areas
Age-standardised avoidable mortality rates by sex and decile, England, 2018
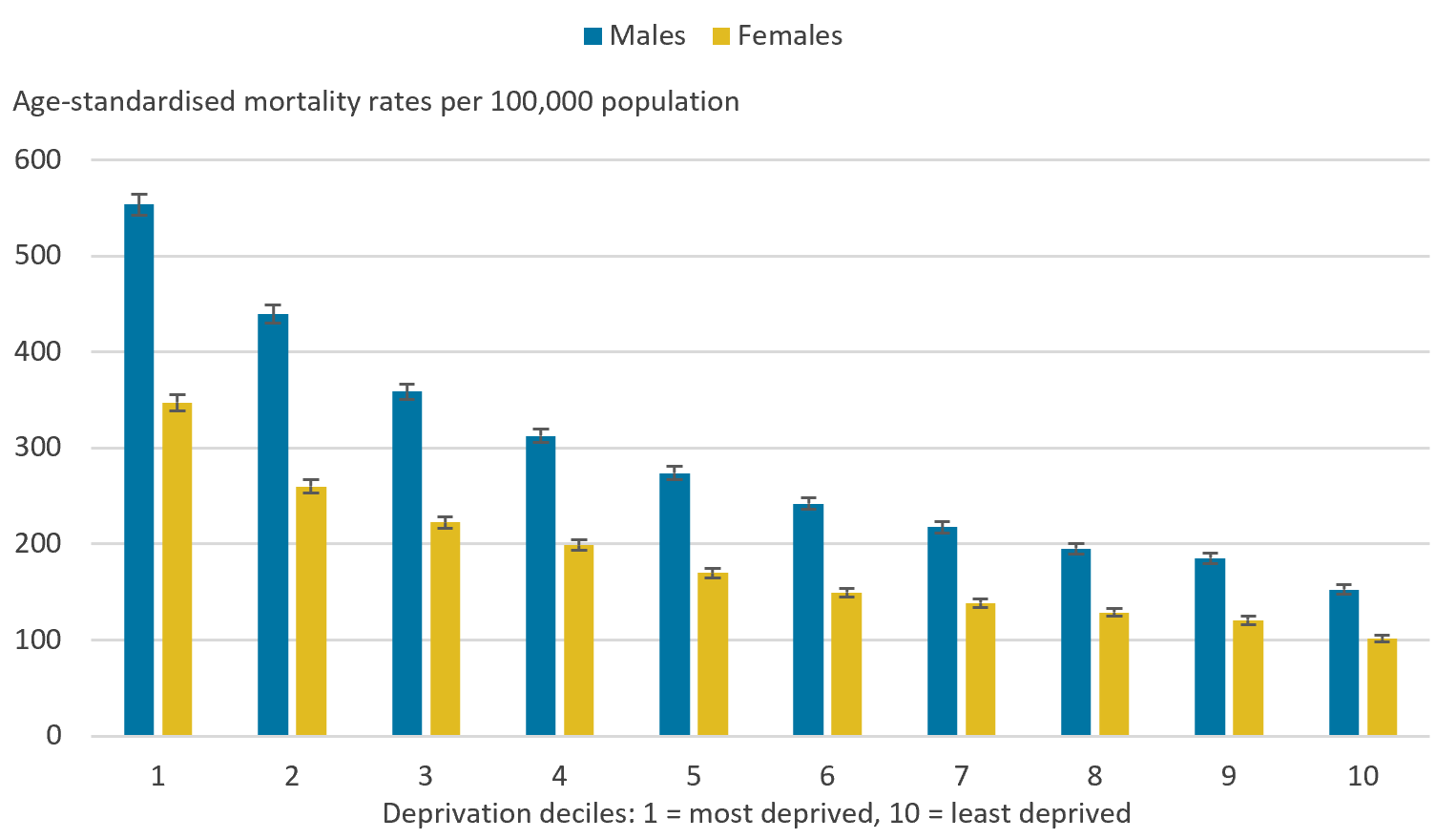
Source: Office for National Statistics - Deaths registered in England
Notes:
Figures are for deaths registered in 2018.
Figures for England exclude deaths of non-residents.
Age-standardised mortality rates are expressed per 100,000 population and standardised to the 2013 European Standard Population. Age-standardised mortality rates are used to allow comparison between populations that may contain different proportions of people of different ages.
Deprivation deciles are based on the Index of Multiple Deprivation (IMD) which is the official measure of relative deprivation. 2018 data is based on IMD 2019.
Decile 1 represents the most deprived areas and decile 10 represents the least deprived areas.
Download this image Figure 1: Males and females living in the most deprived areas had statistically significant higher avoidable mortality rates than those living in the least deprived areas
.png (39.3 kB) .xlsx (19.6 kB)Between 2001 and 2018, avoidable mortality rates statistically significantly decreased for males and females living in the most and least deprived areas of England, with the greatest declines observed in the most deprived areas (Figure 2). In the latest years, declines have slowed with instances of rates increasing. However, the overall decreases across the data time series led the absolute gap in avoidable mortality between the most and least deprived areas to be narrower in 2018 compared with 2001 for both sexes.
Preventable and treatable mortality rates also followed a similar pattern to avoidable mortality, with statistically significant decreases for males and females living in the most and least deprived areas between 2001 and 2018. This resulted in the absolute gap in treatable and preventable mortality to be narrower in 2018 compared with 2001. Data for these measures can be found in the accompanying datasets.
Figure 2: Avoidable mortality rates for males and females living in the most and least deprived areas statistically significantly decreased between 2001 and 2018
Age-standardised avoidable mortality rates by sex and selected deciles, England, 2001 to 2018
Source: Office for National Statistics - Deaths registered in England
Notes:
Figures are for deaths registered in each calendar year.
Figures for England exclude deaths of non-residents.
Age-standardised mortality rates are expressed per 100,000 population and standardised to the 2013 European Standard Population. Age-standardised mortality rates are used to allow comparison between populations that may contain different proportions of people of different ages.
Deprivation deciles are based on the Index of Multiple Deprivation (IMD) which is the official measure of relative deprivation. IMD 2004 was used for data years 2001 to 2003, IMD 2007 was used for years 2004 to 2006, IMD 2010 was used for years 2007 to 2010, IMD 2015 was used for years 2011 to 2015 and IMD 2019 was used for years 2016 to 2018.
Decile 1 represents the most deprived areas and decile 10 represents the least deprived areas.
Download this chart Figure 2: Avoidable mortality rates for males and females living in the most and least deprived areas statistically significantly decreased between 2001 and 2018
Image .csv .xlsFigure 3 illustrates the improvements in avoidable mortality rates across three discrete time periods spanning six years: 2001 and 2006, 2007 and 2012, and 2013 and 2018. The percentage change between 2013 and 2018 was notably smaller than the previous two time periods, with the rate for females living in the most deprived areas worsening, with a 4.5% increase in avoidable deaths. This contrasts with females living in the least deprived areas, where avoidable mortality rates reduced by 8.5% in the later period.
These findings support and are consistent with the marked slowdown of improvement in mortality rates in the latest period, which was also found in the recent changing trends in mortality analysis and health state life expectancy by national deprivation deciles releases. These findings also show that even in periods where avoidable mortality was reducing quickly, rates reduced more rapidly in the least deprived areas compared with the most.
Overall, male and female avoidable mortality rates have decreased since 2001, however, improvements in male avoidable mortality rates exceeded those of females. Similar sex-specific improvements were also observed in health state life expectancy where life expectancy changes were generally more favourable for males compared with females.
Figure 3: Greater improvements in avoidable mortality rates were seen between 2001 and 2012, for both males and females
Percentage change in age-standardised avoidable mortality rates by sex and decile, England, between 2001 and 2006, 2007 and 2012 and 2013 and 2018
Source: Office for National Statistics - Deaths registered in England
Notes:
Percentage change in avoidable mortality is calculated by subtracting the earlier mortality rate from the later mortality rate for each time period, before dividing by the earlier mortality rate. This is expressed as a percentage.
Figures are for deaths registered in each calendar year.
Figures for England exclude deaths of non-residents.
Deprivation deciles are based on the Index of Multiple Deprivation (IMD) which is the official measure of relative deprivation. IMD 2004 was used for data years 2001 to 2003, IMD 2007 was used for years 2004 to 2006, IMD 2010 was used for years 2007 to 2010, IMD 2015 was used for years 2011 to 2015 and IMD 2019 was used for years 2016 to 2018.
Decile 1 represents the most deprived areas and decile 10 represents the least deprived areas.
Download this chart Figure 3: Greater improvements in avoidable mortality rates were seen between 2001 and 2012, for both males and females
Image .csv .xls4. Socioeconomic inequalities in avoidable mortality by cause
Causes of avoidable mortality can be categorised into seven broad cause groups. This section has focused on four of these broad causes:
- diseases of the circulatory system
- diseases of the respiratory system
- alcohol-related and drug-related disorders
- injuries
Data for all broad cause groups are available in the accompanying datasets.
Diseases of the circulatory system
Between 2001 and 2018, avoidable mortality rates for diseases of the circulatory system showed a statistically significant decrease for males and females living in both the most and least deprived areas of England (Figure 4).
The largest absolute decreases were observed in the most deprived areas, falling by 164.3 deaths per 100,000 males and 80.0 deaths per 100,000 females. This is in comparison with those living in the least deprived areas, with decreases of 73.3 deaths per 100,000 males and 34.3 deaths per 100,000 females. These overall decreases led to a narrowing in the absolute gap between the most and least deprived areas in 2018 compared with 2001.
Even though avoidable mortality rates caused by diseases of the circulatory system have statistically significantly decreased between 2001 and 2018, avoidable mortality rates in 2018 for those living in the most deprived areas remained statistically significantly higher compared with those living in the least deprived areas (3.6 times higher for males and 4.4 times higher for females). Additionally, avoidable mortality rates for males remain statistically significantly higher than for females living in the same decile.
Between 2001 and 2011, avoidable mortality rates for males and females living in the most and least deprived areas generally decreased year-on-year, with an overall statistically significant decline. In contrast, between 2011 and 2018, a pronounced slowing down in improvement was observed; however, declines remained statistically significant for males living in the most deprived areas and males and females living in the least deprived areas.
Figure 4: Avoidable mortality rates decreased for diseases of the circulatory system between 2001 and 2018 in the most and least deprived areas
Age-standardised avoidable mortality rates for diseases of the circulatory system by sex and selected deciles, England, 2001 to 2018
Source: Office for National Statistics - Deaths registered in England
Notes:
Figures are for deaths registered in each calendar year.
Figures for England exclude deaths of non-residents.
Age-standardised mortality rates are expressed per 100,000 population and standardised to the 2013 European Standard Population. Age-standardised mortality rates are used to allow comparison between populations that may contain different proportions of people of different ages.
Deprivation deciles are based on the Index of Multiple Deprivation (IMD) which is the official measure of relative deprivation. IMD 2004 was used for data years 2001 to 2003, IMD 2007 was used for years 2004 to 2006, IMD 2010 was used for years 2007 to 2010, IMD 2015 was used for years 2011 to 2015 and IMD 2019 was used for years 2016 to 2018.
Decile 1 represents the most deprived areas and decile 10 represents the least deprived areas.
Download this chart Figure 4: Avoidable mortality rates decreased for diseases of the circulatory system between 2001 and 2018 in the most and least deprived areas
Image .csv .xlsDiseases of the respiratory system
Avoidable mortality rates for diseases of the respiratory system were sharply contrasting between those living in the most and least deprived areas of England, with rates in the former 6.9 times higher for males and 7.8 times higher for females in 2018 (Figure 5).
Between 2001 and 2018, avoidable mortality rates for males living in the most deprived areas have fluctuated, with an overall non-significant increase of 1.1%. Since 2012, however, mortality rates have statistically significantly increased by 18.0%. In contrast, avoidable mortality rates for males living in the least deprived areas statistically significantly decreased between 2001 and 2018. This resulted in the absolute gap between those living in the most and least deprived areas to be wider in 2018 than 2001.
Like males, avoidable mortality rates for females living in the most deprived areas have fluctuated between 2001 and 2018, with an overall statistically significant increase from 63.1 deaths per 100,000 females in 2001 to 75.8 deaths per 100,000 females in 2018. This contrasts with females living in the least deprived areas where there has been much less volatility, with an overall statistically significant decrease. These contrasting observations resulted in the absolute gap between females living in the most and least deprived areas to be wider in 2018 than 2001.
The lack of health improvement in these diseases among deprived populations has caused the inequality to grow. The substantially higher rates observed in the most deprived areas compared with the least deprived areas can be linked to differential smoking prevalence and exposure to air pollution, both of which are higher in more deprived areas, and these two factors combined have a role in increasing risk of respiratory-related mortality.
Figure 5: The gap between avoidable mortality rates for diseases of the respiratory system between the most and least deprived areas was wider in 2018 than 2001
Age-standardised avoidable mortality rates for diseases of the respiratory system by sex and selected deciles, England, 2001 to 2018
Source: Office for National Statistics - Deaths registered in England
Notes:
Figures are for deaths registered in each calendar year.
Figures for England exclude deaths of non-residents.
Age-standardised mortality rates are expressed per 100,000 population and standardised to the 2013 European Standard Population. Age-standardised mortality rates are used to allow comparison between populations that may contain different proportions of people of different ages.
Deprivation deciles are based on the Index of Multiple Deprivation (IMD) which is the official measure of relative deprivation. IMD 2004 was used for data years 2001 to 2003, IMD 2007 was used for years 2004 to 2006, IMD 2010 was used for years 2007 to 2010, IMD 2015 was used for years 2011 to 2015 and IMD 2019 was used for years 2016 to 2018.
Decile 1 represents the most deprived areas and decile 10 represents the least deprived areas.
Download this chart Figure 5: The gap between avoidable mortality rates for diseases of the respiratory system between the most and least deprived areas was wider in 2018 than 2001
Image .csv .xlsAlcohol-related and drug-related disorders
Between 2001 and 2018, avoidable mortality rates for deaths caused by alcohol-related and drug-related disorders have remained statistically significantly higher for those living in the most deprived areas compared with the least deprived areas (6.2 times higher for males and 5.2 times higher for females in 2018) (Figure 6).
The mortality rates for those living in the most deprived areas have statistically significantly increased between 2001 and 2018 by 8.0 deaths per 100,000 males and 7.8 deaths per 100,000 females. Similarly, those living in the least deprived areas also saw an increase in avoidable mortality rates, however, these increases were not significant. The observed increases resulted in the absolute gap between the most and least deprived areas in England to be wider in 2018 compared with 2001.
Figure 6: Avoidable mortality rates for alcohol and drug related disorders statistically significantly increased in the most deprived areas between 2001 and 2018
Age-standardised avoidable mortality rates for alcohol-related and drug-related disorders by sex and selected deciles, England, 2001 to 2018
Source: Office for National Statistics - Deaths registered in England
Notes:
Figures are for deaths registered in each calendar year.
Figures for England exclude deaths of non-residents.
Age-standardised mortality rates are expressed per 100,000 population and standardised to the 2013 European Standard Population. Age-standardised mortality rates are used to allow comparison between populations that may contain different proportions of people of different ages.
Deprivation deciles are based on the Index of Multiple Deprivation (IMD) which is the official measure of relative deprivation. IMD 2004 was used for data years 2001 to 2003, IMD 2007 was used for years 2004 to 2006, IMD 2010 was used for years 2007 to 2010, IMD 2015 was used for years 2011 to 2015 and IMD 2019 was used for years 2016 to 2018.
Decile 1 represents the most deprived areas and decile 10 represents the least deprived areas.
Download this chart Figure 6: Avoidable mortality rates for alcohol and drug related disorders statistically significantly increased in the most deprived areas between 2001 and 2018
Image .csv .xlsInjuries
Between 2001 and 2018, avoidable mortality rates for injuries decreased for both sexes living in the most and least deprived areas of England, however, these decreases were only statistically significant for males living in the most deprived areas, with a decline of 11.2 deaths per 100,000 males (Figure 7).
The majority of the decline observed for males living in the most deprived areas occurred between 2001 and 2011, with a statistically significant decrease, followed by a non-significant decrease between 2011 and 2018. Despite this slowdown, the absolute gap between males living in the most and least deprived areas was narrower in 2018 compared with 2001. The absolute gap between females living in the most and least deprived areas was also narrower in 2018.
Figure 7: Avoidable mortality rates for injuries for males living in the most deprived areas statistically significantly decreased between 2001 and 2018
Age-standardised avoidable mortality rates for injuries by sex and selected deciles, England, 2001 to 2018
Source: Office for National Statistics - Deaths registered in England
Notes:
Figures are for deaths registered in each calendar year.
Figures for England exclude deaths of non-residents.
Age-standardised mortality rates are expressed per 100,000 population and standardised to the 2013 European Standard Population. Age-standardised mortality rates are used to allow comparison between populations that may contain different proportions of people of different ages.
Deprivation deciles are based on the Index of Multiple Deprivation (IMD) which is the official measure of relative deprivation. IMD 2004 was used for data years 2001 to 2003, IMD 2007 was used for years 2004 to 2006, IMD 2010 was used for years 2007 to 2010, IMD 2015 was used for years 2011 to 2015 and IMD 2019 was used for years 2016 to 2018.
Decile 1 represents the most deprived areas and decile 10 represents the least deprived areas.
Download this chart Figure 7: Avoidable mortality rates for injuries for males living in the most deprived areas statistically significantly decreased between 2001 and 2018
Image .csv .xls5. The Slope Index of Inequality (SII) in avoidable mortality
The Slope Index of Inequality (SII) is used to assess the absolute inequality in avoidable mortality and represents the difference between the hypothetical "most" and "least" deprived areas on the deprivation scale taking into account inequality across all adjacent deciles.
Between 2001 and 2018, there was a statistically significant decrease in the SII in avoidable deaths, shrinking from 522.6 deaths per 100,000 males to 396.7 deaths per 100,000 males and from 268.7 deaths per 100,000 females to 234.8 deaths per 100,000 females. Specifically, this indicates that in 2018 there were 396.7 additional deaths per 100,000 males living in the most deprived areas of England compared with the least deprived areas and 234.8 additional deaths per 100,000 females living in the most deprived areas compared with the least (Figure 8).
Between 2001 and 2011, reductions of the inequality in avoidable mortality were evident, with statistically significant decreases observed for both males and females. However, since 2011, a slowing in improvement has been observed, with a non-significant decrease for males and a non-significant increase for females.
Overall, these findings highlight that the statistically significant improvements seen between 2001 and 2018 in narrowing the gap in inequality between the most and least deprived areas of England, were largely driven by decreases in risk of death caused by diseases of the circulatory system during the period 2001 to 2011 in the most deprived areas.
Figure 8: The Slope Index of Inequality (SII) in avoidable mortality was statistically significantly lower in 2018 compared with 2001
Trend in the Slope Index of Inequality (SII) for avoidable mortality by sex, England, 2001 to 2018
Source: Office for National Statistics - Deaths registered in England
Notes:
Figures are for deaths registered in each calendar year.
Figures for England exclude deaths of non-residents.
The SIope Index of Inequality (SII) is reported as a positive value to demonstrate increasing mortality rates with increasing deprivation. However, because the relative rank ranges from 0 (most deprived) to 100 (least deprived) the actual SII is negative.
Download this chart Figure 8: The Slope Index of Inequality (SII) in avoidable mortality was statistically significantly lower in 2018 compared with 2001
Image .csv .xls6. Socioeconomic inequalities in avoidable mortality in England data
Socioeconomic inequalities in avoidable mortality: England analysis
Dataset | Released 10 July 2020
Annual age-standardised mortality rates by deprivation decile, sex and cause as well as absolute (Slope Index of Inequality) measures of inequality in England.
7. Glossary
Preventable mortality
Preventable mortality refers to causes of death that can be mainly avoided through effective public health and primary prevention interventions (that is, before the onset of diseases or injuries, to reduce incidence).
Treatable mortality
Treatable mortality refers to causes of death that can be mainly avoided through timely and effective healthcare interventions, including secondary prevention and treatment (that is, after the onset of disease, to reduce case-fatality).
Avoidable mortality
Avoidable mortality refers to deaths that are preventable or treatable.
Statistical significance
The term "significant" refers to statistically significant changes or differences. Significance is determined by the 95% confidence intervals, where non-overlapping confidence intervals between figures demonstrate that the difference is unlikely to be because of random fluctuation.
Age-standardised mortality rates
Age-standardised mortality rates are used to allow comparisons between populations, which may contain different proportions of people of different ages.
Slope Index of Inequality (SII)
The SII models the absolute inequality (the difference between the hypothetical most and least deprived populations) in avoidable mortality using weighted linear regression, which takes account of the inequality across all adjacent deciles of relative deprivation, rather than focusing only on the differencing of the two extremes.
Nôl i'r tabl cynnwys8. Measuring the data
This article looks at the socioeconomic inequalities in avoidable mortality in England from 2001 to 2018. The analyses use age-standardised mortality rates by deprivation decile, sex and cause as well as absolute (Slope Index of Inequality) measures of inequality. Figures are calculated using death registration data for England held by the Office for National Statistics (ONS).
Defining avoidable mortality
With advances in medical technology and wider public health interventions, deaths from conditions previously not avoidable may have since become avoidable. This means the avoidable mortality definition requires review and, if appropriate, revisions.
In 2017, an Organisation for Economic Co-operation and Development (OECD) working group was set up to review the definitions of avoidable mortality used internationally with a remit to create a harmonised definition. The group proposed a new definition of avoidable mortality (PDF, 688KB) and in 2019, the ONS ran a public consultation (DOC, 730KB) to review this definition. As a result of the consultation, it was agreed the ONS would implement the new international avoidable mortality definition (DOC, 421KB) to ensure our statistics are comparable. The new definition has been implemented from data year 2001 onwards. Please note that under the new avoidable mortality definition, there is an upper age limit of 74 years for all causes of death.
Our definition of avoidable mortality is different to the measure of avoidable deaths in hospital, which NHS Trusts in England are required to publish figures on. We use a defined set of underlying causes of death that have been approved through consultation with users and expert guidance. It includes conditions where it is reasonable to expect deaths to be avoided through good quality healthcare, even after the condition has developed (treatable mortality), as well as those where it is possible to prevent the condition from occurring in the first place (incidence reduction) through wider public health interventions, such as those targeted at reducing the incidence of smoking (preventable mortality).
The avoidable deaths in hospital measure is based on a record review of a sample of deaths deemed to be the result of problems in care. Avoidable deaths in hospital data are not intended to be comparable and are not currently collated centrally.
Socioeconomic deprivation
Socioeconomic deprivation is measured using England's Index of Multiple Deprivation (IMD), which provides an overall relative measure of deprivation for each Lower layer Super Output Area (LSOA). An LSOA is a small area with an average population of 1,500 people. The overall deprivation scores are ranked for all LSOAs within a country and can be divided into 10 groups (deciles) where decile 1 represents the most deprived LSOAs and decile 10 represents the least deprived LSOAs. The IMD is a score based on the area as a whole and not everyone within a LSOA necessarily experiences the same level or type of deprivation.
Different versions of the IMD were used for this time series:
IMD 2004 was used for data years 2001 to 2003
IMD 2007 was used for data years 2004 to 2006
IMD 2010 was used for data years 2007 to 2010
IMD 2015 was used for data years 2011 to 2015
IMD 2019 was used for data years 2016 to 2018
Early access for quality assurance purposes
We provide early access for quality assurance to a small number of people working in other government bodies. This is for general comment on the plausibility of our findings. However, the ONS itself independently produces these statistics, including determining the focus, content, commentary, illustration and interpretation of the measures presented in this article.
More quality and methodology information on strengths, limitations, appropriate uses, and how the data were created is available in the Socioeconomic inequalities in avoidable mortality QMI.
Nôl i'r tabl cynnwys9. Strengths and limitations
The strengths of the socioeconomic inequalities in avoidable mortality bulletin include:
data are compiled using information supplied when a death is registered, which gives complete population coverage and ensures the estimates are of high precision and representative of the underlying population at risk
coding for cause of death is carried out according to the World Health Organization (WHO) International Classification of Diseases ICD-10 and internationally agreed rules
the implementation of the new international avoidable mortality definition (DOC, 421KB) means our statistics are internationally comparable
The limitations of the socioeconomic inequalities in avoidable mortality bulletin include:
in a very small number of cause of death breakdowns, the number of deaths is either too small to report an age-standardised rate or too small to report a rate with reliability; it is our practice not to calculate rates based on fewer than 10 deaths and rates based on 10 to 19 deaths are marked with a "u" to warn users that their reliability is low
provisional data was not used for this article therefore the time series is not fully up to date

