Cynnwys
- Main points
- Statistician’s comment
- Things you need to know about this release
- Excess winter deaths increased in 2016 to 2017 compared with 2015 to 2016 but did not exceed the winter 2014 to 2015 peak
- Pronounced increase in mortality seen over the winter months
- Females and the elderly were most affected by excess winter mortality
- Predominant strain of influenza in winter 2016 to 2017 impacted the elderly most
- Respiratory disease caused most excess winter deaths
- Relationship between excess winter mortality and temperature is complex
- All English regions observed significant increases in EWM indices between winter periods 2015 to 2016 and 2016 to 2017
- Local authorities demonstrate large variation in EWM across time
- What causes excess winter mortality?
- Links to related statistics
- Quality and methodology
1. Main points
In the 2016 to 2017 winter period, there were an estimated 34,300 excess winter deaths (EWDs) in England and Wales, which represents an excess winter mortality (EWM) index of 20.9%.
Although there has been an increase in EWDs, the number of EWDs does not exceed the peak that was observed in the 2014 to 2015 winter period; however, it was the second highest over the last five winter periods.
Females and the elderly were most affected by excess winter mortality in the 2016 to 2017 winter period.
Over one-third of all excess winter deaths were caused by respiratory diseases in England and Wales in 2016 to 2017.
All of the English regions observed significant increases in the excess winter mortality index between winter periods 2015 to 2016 and 2016 to 2017, whereas excess winter mortality for Wales remained stable.
2. Statistician’s comment
“Whilst there has been an increase in excess winter deaths in England and Wales making the total the second highest over the last five winter periods, the number does not exceed the peak that was observed in the 2014 to 2015 winter period. The increase is likely due to the predominant strain of flu prevalent during the 2016 to 2017 winter, which had greater impact on the elderly than the young.”
Jodie Withers, Health Analysis and Life Events, Office for National Statistics
Nôl i'r tabl cynnwys3. Things you need to know about this release
In common with other countries, more people die in the winter than in the summer in England and Wales. This statistical bulletin presents provisional figures for excess winter deaths (EWD) and also the excess winter mortality (EWM) index in England and Wales for the winter period 2016 to 2017 and final figures for the winter period 2015 to 2016. Historical trends from winter of 1950 to 1951 onwards are also provided for comparison. Figures are presented by sex, age, region and cause of death. Information on temperature and influenza incidence is also given to add context to the mortality figures.
Method for calculating excess winter mortality
Excess winter deaths (EWD)
Johnson and Griffiths (2003) investigated seasonal mortality and reported that historically, above average mortality is typically seen between December and March (PDF, 98KB) in England and Wales. Therefore, our standard method defines the winter period as December to March and compares the number of deaths that occurred in this winter period with the average number of deaths occurring in the preceding August to November and the following April to July. The calculation used is:
This produces the number of excess winter deaths (EWDs). Provisional EWD figures are produced for the most recent winter using special estimation methods (see the “How the output is created” section of the Quality and Methodology Information report), and so are rounded to the nearest 100. Final EWD figures for the previous winter are rounded to the nearest 10.
Excess winter mortality (EWM) index
The EWM index is calculated so that comparisons can be made between sexes, age groups and regions and is calculated as the number of excess winter deaths divided by the average non-winter deaths:
The EWM index is presented with 95% confidence intervals, which are calculated as:
The EWM index shows the percentage of extra deaths that occurred in the winter and is reported to one decimal place.
More details about how EWM is calculated and how to interpret and use confidence intervals are available in the Excess Winter Mortality in England and Wales Quality and Methodology Information report.
Nôl i'r tabl cynnwys4. Excess winter deaths increased in 2016 to 2017 compared with 2015 to 2016 but did not exceed the winter 2014 to 2015 peak
In the 2016 to 2017 winter period, there were an estimated 34,300 excess winter deaths (EWDs) in England and Wales, which has increased since the 2015 to 2016 winter period by around 39.5%. This represents an excess winter mortality (EWM) index of 20.9%, which means that 20.9% more deaths occurred in the winter months compared with the non-winter months in 2016 to 2017. Although there has been an increase in EWDs in 2016 to 2017 of almost two-fifths, the number does not exceed the recent peak of deaths that was observed in the 2014 to 2015 winter period, which was exceptionally large compared with recent reference periods in the 21st century (see Figure 1).
Figure 1: Excess winter deaths and five-year central moving average, England and Wales, between 1950 to 1951 and 2016 to 20171,2,3,4
Source: Office for National Statistics
Notes:
- EWD figures are based on deaths occurring in each period (August through to the following July). Numbers of deaths from January to July 2017 are provisional, and have been adjusted to take account of late registrations (see Excess Winter Mortality Quality and Methodology Information document).
- Figures for the latest winter are provisional and are rounded to the nearest 100, figures for all other winters are final and are rounded to the nearest 10.
- Central moving averages were calculated using the winter period of interest, along with the two winter periods before and two periods after.
- Data include non-residents who died in England or Wales.
Download this chart Figure 1: Excess winter deaths and five-year central moving average, England and Wales, between 1950 to 1951 and 2016 to 2017^1,2,3,4^
Image .csv .xlsThe increase in EWDs in 2016 to 2017 can partially be explained by the levels of excess all-cause mortality (meaning total number of deaths due to all causes during the winter months), which were elevated compared with 2015 to 2016, particularly in the elderly. However, all-cause mortality in the elderly was lower than the 2014 to 2015 season in which the same strain of influenza virus dominated (Public Health England, 2017a). In addition, the increase appears large as a lower than average number of EWDs occurred in the 2015 to 2016 period meaning any increase above the five-year average would appear large in comparison with the winter of 2015 to 2016.
It is common to observe large fluctuation in EWDs for which trends over time are often not smooth. Therefore, we present a five-year moving average to smooth out any short-term fluctuations and make the trend over time clearer (see Figure 1). Overall, historical trends in EWDs in England and Wales show that the steady decline in EWDs since the 1950 to 1951 winter period has levelled off in recent years, with the most recent estimates more consistent with a slight five-year average rise since 2012 to 2013.
Nôl i'r tabl cynnwys5. Pronounced increase in mortality seen over the winter months
For the 2016 to 2017 winter period, the peak in daily deaths occurred towards the beginning of January 2017. This is earlier than the previous winter period where the peak occurred towards the end of January 2016. The pattern observed this winter is more similar to 2014 to 2015 and winters prior to this period. The peak in mortality at the beginning of January 2017 can be partly explained by moderate levels of a dominant strain of influenza A(H3N2) activity (PDF, 1.35MB) peaking in week 1 of 2017 (Public Health England, 2017a). The peak could also be partly explained by temperature as it was found that temperatures during the winter months of 2016 to 2017 were colder than the winter months of the previous year (2015 to 2016). The minimum daily temperatures during the first week of January 2017 were also lower than January 2016.
In 2016 to 2017, the number of daily deaths exceeding the five-year average was prominent during the winter months. The shape of the distribution is typical as evident in the five-year average (see Figure 2). Of the 365 days in the 2016 to 2017 period, there were 244 days where the number of daily deaths was higher than the five-year average. However, throughout March and April, the number of daily deaths was often lower than the five-year average.
Figure 2: Number of daily deaths and five-year average daily deaths, August 2016 to July 2017, England and Wales1,2,3
Source: Office for National Statistics
Notes:
- Figures are based on deaths occurring each day. Numbers of deaths from January to July 2017 are provisional, and have been adjusted to take account of late registrations (see the Excess Winter Mortality Quality and Methodology Information document).
- Five year averages for each day are calculated using data from the previous five years, excluding the current year.
- Mortality data include non-residents who died in England or Wales.
Download this chart Figure 2: Number of daily deaths and five-year average daily deaths, August 2016 to July 2017, England and Wales^1,2,3^
Image .csv .xlsSimilar to the previous winter (2015 to 2016), there was a noticeable peak during the summer months, this time in June, which has also been reported in the Quarterly Mortality Report for England (ONS, 2017). The peak in number of daily deaths on 19 June 2017 coincided with a period of warmer weather where the daily temperatures were substantially higher than any other days in the preceding weeks and were also higher than the five-year average temperature for these days. Central England daily temperatures from the Met Office Hadley Centre show that the highest temperature of the year was observed on 19 June 2017 with a mean temperature of 21.9 degrees Celsius and maximum temperature of 29.1 degrees Celsius.
Nôl i'r tabl cynnwys6. Females and the elderly were most affected by excess winter mortality
Of the estimated 34,300 EWDs in 2016 to 2017, males comprised 42.4% (14,600 EWDs) and females 57.6% (19,800 EWDs). EWDs are generally higher in females than males, which may partly be explained by the higher proportion of females aged 85 and over compared with males; 64.5% of the population aged 85 and over are female (ONS, 2017).
Figures 3a and 3b show the excess winter mortality (EWM) index for males and females respectively for the last three winter periods by age group. The EWM index describes how many more people died in winter than in non-winter months expressed as a percentage of the average number of deaths in the non-winter months.
For both males and females, the highest EWM index for the winter period 2016 to 2017 was for those aged 85 and over (26.8% and 31.2% respectively). Since the previous winter period, the EWM index has increased significantly for females (from 17.8%), however, this is lower than the 2014 to 2015 winter period (EWM index of 41.8%).
From the winter of 2015 to 2016 to the 2016 to 2017 winter, the EWM index increased significantly across the age groups 65 to 74, 75 to 84 and 85 and over for females, with a significant decline for females aged 0 to 64. For males, the EWM index increased significantly for those aged 75 to 84 and 85 and over, with small declines observed for males aged 0 to 64 and 65 to 74. The decline observed in under-65 year olds could be explained partly by influenza vaccine uptake rates in 2016 to 2017 (PDF, 1.35MB), which were higher than the 2015 to 2016 season in England and Wales (Public Health England, 2017a). Additionally, the decline could also be because the predominant strain of influenza impacted the young more than the elderly during winter 2015 to 2016.
These findings are different to last year for males and females where the EWM indices were similar across age groups. For males and females, those aged 85 and over observed the largest increase in EWDs between 2015 to 2016 and 2016 to 2017, accounting for 45.9% and 63.1% of all EWDs respectively (up from 38.3% and 53.4% respectively).
Overall, for males of all ages, the EWM index increased to 18.0% (up from 13.8% in 2015 to 2016) compared with 23.6% (up from 15.9%) for females of all ages. Figures appear to be closer to the pattern observed in 2014 to 2015 period where there was a larger increase. This can be explained by the same predominant strain of flu impacting the elderly during the winters of 2014 to 2015 and 2016 to 2017, whereas the predominant strain of flu during 2015 to 2016 impacted the young.
Figure 3a: Excess winter mortality index by age group, males, England and Wales, between 2014 to 2015 and 2016 to 20171,2,3,4,5
Source: Office for National Statistics
Notes:
- EWM figures are based on deaths occurring in each period (August through to the following July). Numbers of deaths from January to July 2017 are provisional, and have been adjusted to take account of late registrations (see Excess Winter Mortality Quality and Methodology Information document).
- Figures for the latest winter are provisional and are rounded to the nearest 100, figures for all other winters are final and are rounded to the nearest 10.
- Totals for all ages will not be equal to the sum of the individual age groups due to rounding.
- The excess winter mortality (EWM) index is calculated as excess winter deaths divided by the average non-winter deaths, expressed as a percentage.
- Data include non-residents who died in England or Wales.
Download this chart Figure 3a: Excess winter mortality index by age group, males, England and Wales, between 2014 to 2015 and 2016 to 2017^1,2,3,4,5^
Image .csv .xls
Figure 3b: Excess winter mortality index by age group, females, England and Wales, between 2014 to 2015 and 2016 to 20171,2,3,4,5
Source: Office for National Statistics
Notes:
- EWM figures are based on deaths occurring in each period (August through to the following July). Numbers of deaths from January to July 2017 are provisional, and have been adjusted to take account of late registrations (see Excess Winter Mortality Quality and Methodology Information document).
- Figures for the latest winter are provisional and are rounded to the nearest 100, figures for all other winters are final and are rounded to the nearest 10.
- Totals for all ages will not be equal to the sum of the individual age groups due to rounding.
- The excess winter mortality (EWM) index is calculated as excess winter deaths divided by the average non-winter deaths, expressed as a percentage.
- Data include non-residents who died in England or Wales.
Download this chart Figure 3b: Excess winter mortality index by age group, females, England and Wales, between 2014 to 2015 and 2016 to 2017^1,2,3,4,5^
Image .csv .xls7. Predominant strain of influenza in winter 2016 to 2017 impacted the elderly most
Influenza is a respiratory disease caused by a viral infection that affects the lungs and airways (World Health Organisation, 2008). Influenza infections can become potentially life-threatening when complications such as bacterial pneumonia occur. Those at most risk of developing complications are persons with other underlying health conditions, and the elderly (Public Health England, 2014a) and such complications may result in hospitalisation or death (Public Health England, 2014b). Respiratory disease is one of the leading causes of excess winter deaths (EWDs), where in 2016 to 2017 there were 61.9% more respiratory deaths in the winter months than non-winter months and 36.4% of all EWDs had a respiratory disease as the underlying cause (12,500 respiratory deaths out of 34,300 EWDs). Around four-fifths (80.8%) of respiratory deaths were amongst those aged 75 and older.
Figure 4 plots the weekly number of deaths and weekly influenza-like illness (ILI) consultation rate in primary care from week 31 in 2000 to week 30 in 2017 (where week 1 is the first week of the year). The ILI consultation rates peaked in week 1 of 2017 (20.5 consultations per 100,000 population) occurring earlier than last season where the ILI consultation rate peak occurred in week 11 of 2016. The highest number of weekly deaths in 2016 to 2017 occurred in week 2 of 2017 with 13,297 deaths. Following week 2 of 2017, there was a decline in both weekly deaths and the weekly ILI consultation rate.
The predominant influenza virus during the 2016 to 2017 period was influenza A(H3N2) whose impact was largely seen in older adults. In England, the highest ILI consultation rate appeared to occur in those aged 75 and over (32.1 per 100,000), which reflects the pattern observed in the winter period 2014 to 2015 where observations of influenza A(H3N2) also predominantly affected older adults (PDF, 1.35MB) (Public Health England, 2017a). According to Public Health England, there were increased numbers of care home outbreaks and EWD particularly for those aged 65 and over due to this predominant influenza virus; although less than that observed in 2014 to 2015 where influenza A(H3N2) last dominated.
In comparison, the predominant influenza virus was influenza A(H1N1)pdm09 in the previous winter period (PDF, 1.19MB) (2015 to 2016), which had a noticeable impact on younger adults and children (Public Health England, 2016). One of the reasons for the reduced EWD in 2015 to 2016 was the strain of the influenza virus having less impact on the elderly. Therefore, the increase observed in 2016 to 2017 in EWD was likely affected by this different strain of influenza A(H3N2), which has greater impact on the elderly. Additionally, it was found that there was no significant effectiveness of the influenza vaccination for those aged 65 and over (PDF, 49KB) compounding the likely impact on mortality risk (Public Health England, 2017b).
Figure 4: Weekly deaths from all causes and Royal College of General Practitioners (RCGP) and Public Health Wales (PHW) influenza-like illness (ILI) consultation rates per 100,000 population, England and Wales, 1999 to 20171,2,3,4
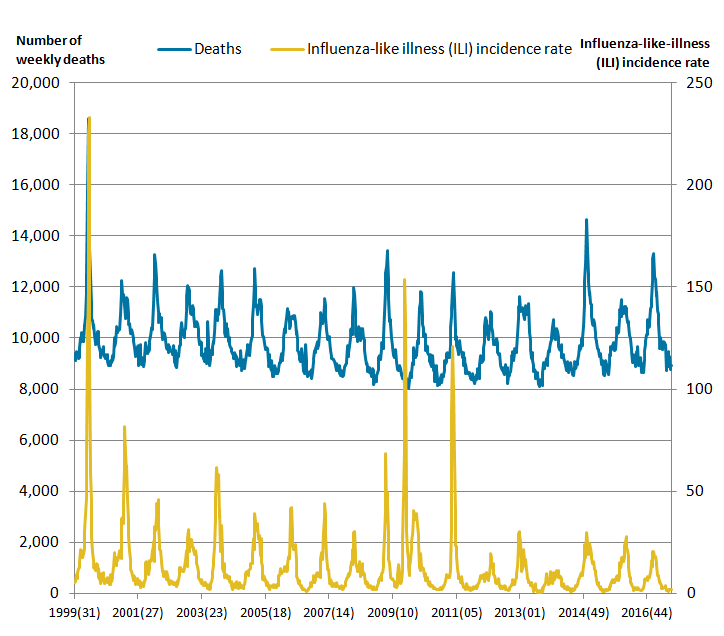
Source: Office for National Statistics, The Royal College of General Practitioners Research and Surveillance Centre and Public Health Wales
Notes:
- Figures are based on deaths occurring each week. Numbers of deaths from January to July 2017 are provisional, and have been adjusted to take account of late registrations (see Excess Winter Mortality Quality and Methodology Information Document).
- The method for calculating ILI rates changed for data from week number 2015(31), so rates from this week onwards are not directly comparable to previous weeks. For more information, see the 'Methodological changes' section of the statistical bulletin.
- Mortality data include non-residents who died in England or Wales.
Download this image Figure 4: Weekly deaths from all causes and Royal College of General Practitioners (RCGP) and Public Health Wales (PHW) influenza-like illness (ILI) consultation rates per 100,000 population, England and Wales, 1999 to 2017^1,2,3,4^
.png (44.4 kB) .xls (79.9 kB)8. Respiratory disease caused most excess winter deaths
Figure 5 presents the excess winter mortality (EWM) index by three leading causes of deaths: circulatory diseases (defined as International Classification of Diseases ICD-10 codes I00 to I99), respiratory diseases (defined as ICD-10 codes J00 to J99) and dementia and Alzheimer’s disease (defined as ICD-10 codes F01, F03 and G30). These three causes were regarded as leading causes of death in England and Wales and in the 2016 to 2017 period accounted for approximately 80% of all excess winter mortality deaths. Of the remaining 20%, one prominent cause was malignant neoplasm of bronchus and lung.
Respiratory diseases were shown to be affected most by seasonal trends. This has generally been the case since the winter of 1991 to 1992, with the exception of the winter of 2000 to 2001 where dementia and Alzheimer’s disease had the greatest EWM index. In 2016 to 2017, there were 61.9% more respiratory deaths in the winter months compared with non-winter months. This equates to 12,500 excess winter deaths caused by respiratory diseases and accounted for 36.4% of all excess winter deaths.
While the EWM index was significantly greater than 2015 to 2016, it remains lower than that seen in 2014 to 2015. Of the 12,500 excess respiratory deaths, pneumonia (specifically ICD-10 code J18) and chronic obstructive pulmonary diseases (specifically ICD-10 code J44) accounted for the largest proportions. The prominence of pneumonia is likely related to the relationship between EWM and a range of bacterial and viral respiratory pathogens including influenza.
Figure 5: Excess winter mortality index, by underlying cause of death, England and Wales, between 2014 to 2015 and 2016 to 20171,2,3,4,5
Source: Office for National Statistics
Notes:
- Underlying cause of death is defined using the International Classification of Diseases, Tenth Revision (ICD-10) using I00-I99 for circulatory diseases, J00-J99 for respiratory diseases and F01, F03 and G30 for dementia and Alzheimer’s disease.
- Figures are based on deaths occurring in each period (August through to the following July). Numbers of deaths from January to July 2017 are provisional, and have been adjusted to take account of late registrations (see Excess Winter Mortality Quality and Methodology Information document).
- The excess winter mortality (EWM) index is calculated as excess winter deaths divided by the average non-winter deaths, expressed as a percentage.
- A more detailed version of Figure 5 showing excess winter mortality, broken down by sex and age group can be found in reference table 1.
- Figures for England and Wales include deaths of non-residents.
Download this chart Figure 5: Excess winter mortality index, by underlying cause of death, England and Wales, between 2014 to 2015 and 2016 to 2017^1,2,3,4,5^
Image .csv .xlsFigure 5 shows that the EWM index of circulatory diseases increased from 13.5% (in 2015 to 2016) to 17.7% (in 2016 to 2017); but wasn’t as high as the figure in 2014 to 2015 (23.0%). Circulatory diseases accounted for 7,400 EWDs, representing a fifth of all EWDs (there was a total of 34,300 excess winter deaths). The number dying from circulatory diseases remained quite high throughout the year, therefore the seasonal differences tend to be lower than respiratory diseases, and dementia and Alzheimer’s disease.
In the winter of 2016 to 2017, there were 39.3% more deaths from dementia and Alzheimer’s disease compared with non-winter months. Of the 34,300 total excess winter deaths, 7,700 had dementia and Alzheimer’s disease as the underlying cause of death (or 22.4%). In 2014 to 2015, EWDs for dementia and Alzheimer’s disease reached a peak of 9,030, which remains among the highest seen. The increase in recent years might partly be down to methodological changes. The reasons for the seasonal pattern in deaths from dementia and Alzheimer's disease are not clear. However, it may be related to the greater vulnerability of people with these conditions to respiratory diseases, difficulties with self-care, and falls, all of which may have greater impact in winter months.
Similar relationships between underlying cause and age can be seen for both males and females. Table 1 in the downloadable dataset is a more detailed version of Figure 5 and shows the number of EWDs and the EWM index in England and Wales between the winters of 1991 to 1992 and 2016 to 2017, by sex and age group for respiratory diseases, circulatory diseases, dementia and Alzheimer’s disease, and injury and poisoning (up to 2015 to 2016). Injury and poisoning are not included in Figure 5 due to the unreliable nature of the latest provisional data (long delays in registration). More information is available in the Quality and Methodology Information report.
Nôl i'r tabl cynnwys9. Relationship between excess winter mortality and temperature is complex
Research has shown that as the temperature gets colder mortality increases, but temperature is only able to explain a part of the variance in excess winter mortality (PDF, 294KB) (Brown et al. 2010).
During the winter period, the months December, January and February had more mean daily deaths compared with the five-year average (see Figure 6). March was the only winter month for which there were fewer mean daily deaths compared with the five-year average. Similar to the last winter period (2015 to 2016), January had the highest mean daily deaths with 1,830 deaths, however, unlike the last winter period; it was higher than the five-year average.
From October to January, below average temperatures were observed with the lowest average daily temperature occurring in January (3.9 degrees Celsius). Colder than average temperatures for these months may partially explain the increase in winter deaths as mean daily deaths were above average between October and January. November was the month with the greatest negative difference from the five-year average in terms of number of deaths and temperature, supporting a relationship between cold weather and excess winter mortality.
Figure 6: Mean number of daily deaths each month and mean monthly temperatures, England and Wales, August 2016 to July 20171,2,3

Source: Office for National Statistics and The Met Office
Notes:
- The mean number of daily deaths is based on deaths occurring in each month. Numbers of deaths from January to July 2017 are provisional, and have been adjusted to take account of late registrations (see Excess Winter Mortality Quality and Methodology Information document).
- Five year averages for each month are calculated using data from the previous five years, excluding the current year.
- Data include non-residents who died in England or Wales.
Download this image Figure 6: Mean number of daily deaths each month and mean monthly temperatures, England and Wales, August 2016 to July 2017^1,2,3^
.png (48.3 kB) .xls (31.7 kB)Excess winter deaths (EWDs) in 2016 to 2017 were of a similar level to those observed in 2012 to 2013. Over the past decade, EWDs have fluctuated with large declines often following unusually high EWD, as was recently observed between winter periods 2014 to 2015 and 2015 to 2016. The majority of winter periods experienced between 20,000 and 30,000 EWDs, with the most recent winter period experiencing in excess of 30,000 EWDs (see Figure 7a).
Figure 7 also demonstrates a weak relationship between temperature and EWDs. Increased excess winter deaths are not always coupled with unusually cold winters and conversely winters with relatively few excess winter deaths are not always coupled with milder winter temperatures indicating that factors other than temperaure, such as influenza, are driving trends in excess winter mortality. However, the use of mean temperature for the four-month period may disguise days of exceptionally cold temperatures that increase risk in the following days, even though the temperature has reverted to more modest values.
Figure 7: Excess winter deaths and average winter temperature, England and Wales, between 1999 to 2000 and 2016 to 20171,2,3,4
Source: Office for National Statistics and The Met Office
Notes:
- EWD figures are based on deaths occurring in each period (August through to the following July). Numbers of deaths from January to July 2017 are provisional, and have been adjusted to take account of late registrations (see Excess Winter Mortality Quality and Methodology Information Document).
- Figures for the latest winter are provisional and are rounded to the nearest 100, figures for all other winters are final and are rounded to the nearest 10.
- Mean winter temperature is calculated using average monthly temperatures from December to March.
- Data include non-residents who died in England or Wales.
Download this chart Figure 7: Excess winter deaths and average winter temperature, England and Wales, between 1999 to 2000 and 2016 to 2017^1,2,3,4^
Image .csv .xls10. All English regions observed significant increases in EWM indices between winter periods 2015 to 2016 and 2016 to 2017
Figures 8a and 8b show excess winter mortality indices for the regions of England and for Wales for each of the last three winter periods. Of the English regions and Wales, the highest EWM index in 2016 to 2017 was Yorkshire and The Humber with 23.8%, which was followed by East of England with 23.0%. Both Yorkshire and The Humber and East of England along with East Midlands, London and South East were significantly higher compared with the England and Wales average (20.9%).
Notably, the lowest EWM index was in Wales (17.6%), which remained relatively stable compared with the previous winter period (2015 to 2016) where Wales had the largest EWM index at 17.4%. The increase in EWDs between 2015 to 2016 and 2016 to 2017 for England and Wales was therefore largely driven by England. Overall, all of the English regions observed significant increases in their EWM indices between winter periods 2015 to 2016 and 2016 to 2017. However, none of the English regions had an EWM index higher than that observed in the 2014 to 2015 winter period. Overall, Figure 8b shows that there was no consistent pattern in EWM over time for the English regions and Wales.
Figure 8a: Excess winter mortality (EWM) for regions of England, and Wales, winter period 2016 to 20171,2,3,4
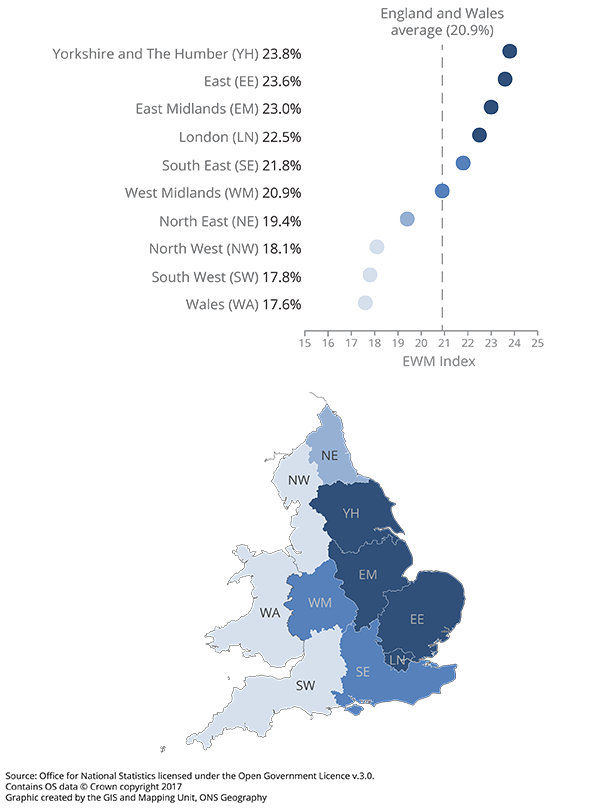
Source: Office for National Statistics licensed under the Open Government Licence v.3.0. Contains OS data © Crown copyright 2017 Graphic created by the GIS and Mapping Unit, ONS Geography
Notes:
- EWM figures are based on deaths occurring in each period. Numbers of deaths from January to July 2017 are provisional, and have been adjusted to take account of late registrations (see Excess Winter Mortality Quality and Methodology Information document).
- The excess winter mortality (EWM) index is calculated as excess winter deaths divided by the average non-winter deaths, expressed as a percentage.
- Figures for the English regions and Wales only include deaths from those usually resident in those areas. The figure for England and Wales combined includes deaths from those not usually resident in England or Wales.
- Based on boundaries as of August 2017.
Download this image Figure 8a: Excess winter mortality (EWM) for regions of England, and Wales, winter period 2016 to 2017^1,2,3,4^
.png (126.7 kB) .xls (32.3 kB)
Figure 8b: Excess winter mortality index for regions of England, and Wales, between 2014 to 2015 and 2016 to 20171,2,3,4
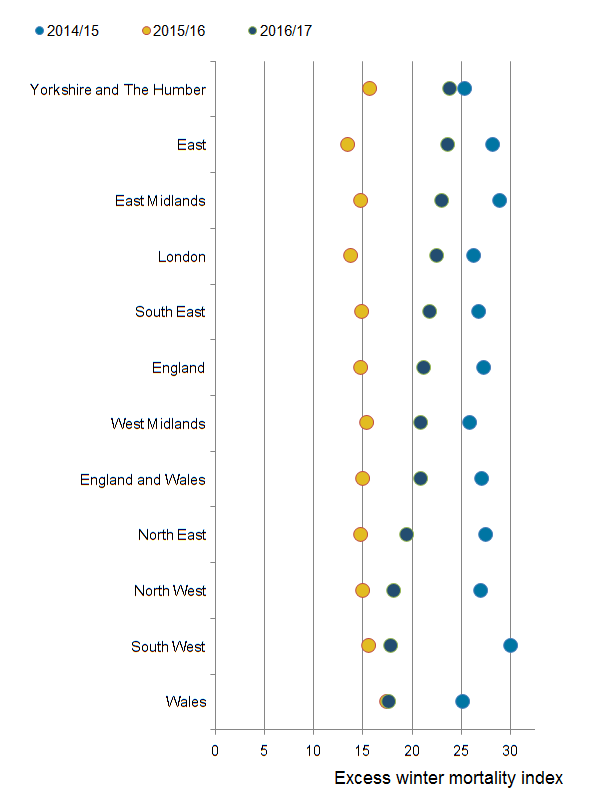
Source: Office for National Statistics
Notes:
- EWM figures are based on deaths occurring in each period. Numbers of deaths from January to July 2017 are provisional, and have been adjusted to take account of late registrations (see Excess Winter Mortality Quality and Methodology Information document).
- The excess winter mortality (EWM) index is calculated as excess winter deaths divided by the average non-winter deaths, expressed as a percentage.
- Figures for England, English regions and Wales exclude deaths of persons usually resident in each area. Figures for England and Wales combined also include deaths of non-residents.
- Based on boundaries as of August 2017.
Download this image Figure 8b: Excess winter mortality index for regions of England, and Wales, between 2014 to 2015 and 2016 to 2017^1,2,3,4^
.png (34.6 kB) .xls (32.3 kB)12. What causes excess winter mortality?
A study by Healy (2003) showed that excess winter mortality (EWM) varied widely within Europe. The results show that countries with low winter temperatures in Scandinavia and Northern Europe, such as Finland and Germany, had very low rates of EWM. Conversely, countries with very mild winter temperatures in Southern Europe such as Portugal and Spain had very high rates of EWM. England and Wales both have higher than average EWM and exhibit high variation in seasonal mortality. These results were echoed in a more recent study by Fowler et al (2014).
There are many reasons why countries with milder winter climates have such a high level of winter mortality. For example, people who live in countries with warmer winters tend to take fewer precautions against the cold. The Eurowinter group (1997) reported that compared with people living in countries with cold winters, those from warmer countries were less likely to wear warm protective clothing in cold weather.
Countries with milder winters also tend to have homes with poorer thermal efficiency (for example, fewer homes have cavity wall insulation and double glazing), which makes it harder to keep homes warm during the winter (Healy, 2003). It has been shown that low indoor temperature is associated with higher EWM from cardiovascular disease in England (Wilkinson et al., 2001).
Although EWM is associated with low temperatures, conditions directly relating to cold, such as hypothermia, are not the main cause of EWM. The majority of additional winter deaths are caused by cerebrovascular diseases, ischaemic heart disease, respiratory diseases, and dementia and Alzheimer’s disease. Although cancer causes more than a quarter of all deaths annually, previous research by Johnson and Griffiths (2003) found that there was no clear seasonal pattern for these deaths (PDF, 98KB).
The cold can have various physiological effects, which may lead to death in vulnerable people. Woodhouse et al (1993) reported that colder home temperature was associated with increased blood pressure in older people. The Eurowinter group (1997) noted that cold causes haemoconcentration, which leads to thrombosis and that cold can also lower the immune system’s resistance to respiratory infections. Additionally, the level of influenza circulating in the population increases in winter. In vulnerable groups, for example, in the elderly or those with pre-existing health problems, influenza can lead to life-threatening complications, such as bronchitis or secondary bacterial pneumonia (Public Health England, 2014).
Previous research has shown that although mortality does increase as it gets colder, temperature only explains a small amount of the variance in winter mortality and high levels of EWM can occur during relatively mild winters (PDF, 294KB) (Brown et al, 2010). Curwen and Devis (1988) showed that both temperature and levels of influenza were important predictors of excess winter mortality. The relationship between temperature, influenza and winter mortality is complex.
Nôl i'r tabl cynnwys14. Quality and methodology
The Excess Winter Mortality in England and Wales Quality and Methodology Information report contains important information on:
- the strengths and limitations of the data and how it compares with related data
- uses and users of the data
- how the output was created
- the quality of the output including the accuracy of the data

