1. Main points
- Productivity in publicly funded adult social care services fell by 1.4% in financial year ending (FYE) 2019, as more inputs were used, but quality-adjusted output provided decreased slightly.
- The amount of inputs used in the provision of adult social care increased 1.3% in FYE 2019; this was an increase on the 0.3% growth in FYE 2018.
- Quality-adjusted output fell by 0.1% in FYE 2019 as, while the quantity of services provided increased, output quality fell by more; this followed a previous fall in output of 0.3% in FYE 2018.
- While the 0.9% growth in the quantity of output provided was the fastest since FYE 2016, the output quality reduction of 1.0% in FYE 2019 marked the second consecutive year of falling quality.
- Overall, productivity was 9.2% lower in FYE 2019 than in FYE 1997, meaning 9.2% less output was provided for each unit of input.
- Residential and nursing care, which accounts for nearly one-third of adult social care expenditure, experienced a 2.2% fall in productivity in FYE 2019, reflecting falls in both the quantity and quality of output provided.
2. Productivity
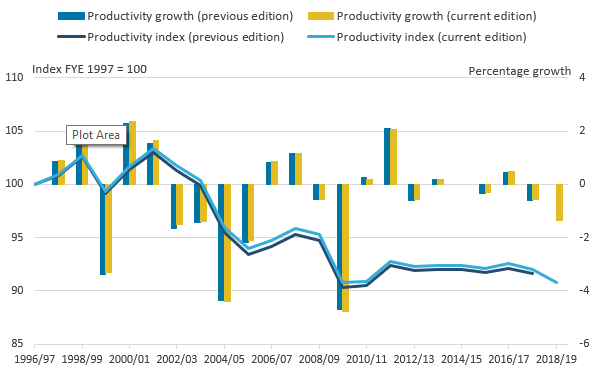
Productivity across publicly funded adult social care (ASC) fell by 1.4% in financial year ending (FYE) 20191, continuing the trend in FYE 2018, when productivity fell by 0.6%.
Over the course of the available time series, from FYE 1997 to FYE 2019, productivity has fallen by 9.2% overall. This means that in FYE 2019, 9.2% less output was provided for each unit of input than it was in FYE 1997.
Figure 1: Publicly funded ASC productivity was 9.2% lower in FYE 2019 than in FYE 1997
Public service adult social care productivity, England, financial year ending (FYE) 1997 to FYE 2019
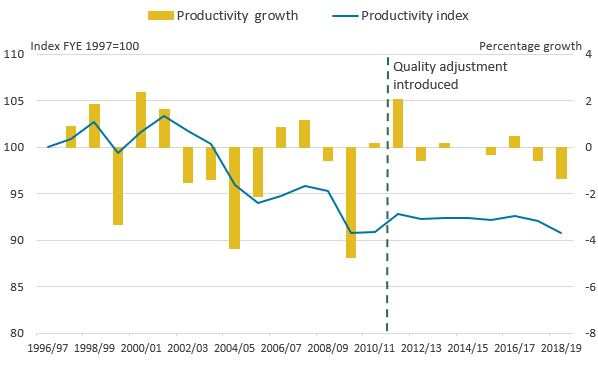
Source: Office for National Statistics
Notes:
- Output is quality adjusted from FYE 2012 onwards. No equivalent data are available to quality adjust output before this.
- No productivity change is calculated for FYE 2015 because of a change of data source between this and the previous year.
Download this image Figure 1: Publicly funded ASC productivity was 9.2% lower in FYE 2019 than in FYE 1997
.png (20.3 kB) .xls (51.2 kB)Understanding the reasons for rises or falls in productivity requires analysis of the growth in output and inputs. Output represents the amount of services provided adjusted for the quality of the service, while inputs represent the amount of resources needed to provide services. Figure 2 shows that the fall in productivity in FYE 2019 is a consequence of ASC output falling at the same time as the amount of inputs used in providing services was increasing. These are the same reasons behind the fall in productivity in FYE 2018.
The fall in output in FYE 2019 was the result of a fall in the quality adjustment to output, rather than a fall in the quantity of output produced, which increased by 0.9%. This means that, while quality-adjusted productivity fell by 1.4%, non-quality-adjusted productivity fell by only 0.4%. More information on the quantity of output is available in Section 4.
Figure 2: There have only been small changes in the level of both inputs and output since FYE 2006
Public service adult social care inputs and output, England, financial year ending (FYE) 1997 to FYE 2019
Source: Office for National Statistics
Notes:
- Output is quality adjusted from FYE 2012 onwards. No equivalent data are available to quality adjust output before this.
Download this image Figure 2: There have only been small changes in the level of both inputs and output since FYE 2006
.PNG (27.5 kB) .xls (52.2 kB)Figure 2 shows that much of the fall in productivity across the whole series can be traced to the period between FYE 2002 and FYE 2006, when there was a large increase in output but an even larger increase in inputs. This means that the amount of resources used in providing ASC services was increasing by more than the quantity of ASC services delivered.
Since FYE 2010, both the quantity of inputs used and output provided have changed little, generally resulting in only small changes in productivity. However, productivity fell in both FYE 2018 and FYE 2019.
Interpreting ASC productivity
These falls in ASC productivity could be because of a deterioration in the efficiency of service provision. However, it is important to consider how clients’ levels of needs (and consequently, the intensity of support they require) may have increased over time.
The ASC output measure partly controls for this by giving different weights for different activities, client age groups, and primary reasons for needing support. The result of these controls is that ASC output in the productivity measure has not fallen as client numbers have (as shown in Figure 9 of Public service productivity: adult social care, England, financial year ending 2018).
However, the lack of data on the level of care clients need prevents us observing and fully controlling for these needs. The National Audit Office, in Adult social care in England: overview (PDF, 636.66KB) points to demographic factors – such as ageing – being responsible for increasing the number of people with high-intensity needs. If those clients are making up an increasing proportion within each primary support need group, the output measure may understate growth and the productivity measure may overstate the fall in productivity.
In line with the Atkinson Review (PDF, 1.08MB) framework for measuring public service productivity, the ASC productivity measure covers publicly funded ASC services, whether provided by local authority or independent sector providers. Controlling for other factors (including service quality), a lower real rate of payment per client made by local authorities to independent sector providers would result in higher productivity, reflecting the service providing more publicly funded output for the publicly funded inputs used.
However, we do not directly observe or control for the effect of public spending per client on the financial position of independent sector providers. A review undertaken by the Competition and Markets Authority (2017) suggests that independent sector providers of residential and nursing care have experienced increased financial pressures, partly because of local authority fees being below full economic cost. One result of this has been an increase in the fees independent sector providers charge to self-funding clients, such as those with wealth above the thresholds for receiving local authority support.
In the productivity measure, lower real local authority fees would result in higher productivity, if other factors (including quality) do not also change. This would be the case even if lower fees also resulted in a worsening in the financial sustainability of care providers. Conversely, the falls in residential and nursing care productivity seen in FYE 2018 and FYE 2019 (Figure 10), could be the result of higher fees funded by additional provisions in the 2017 Spring Budget, with one objective of supporting the financial sustainability of care providers.
Data limitations and the productivity of “directly measured” services
Data limitations mean it is not possible to measure the productivity of every ASC service type in every year using our preferred methodology, and these data limitations differ across the time series.
Because of a change in the data source between FYE 2014 and FYE 2015, it is not possible to measure the change in productivity for any ASC services between these two years. Also, following this change from FYE 2015 onwards, activity data are no longer available to measure output and productivity growth using our preferred “directly measured” methodology for most community care services, such as home care and day care. Instead, output for these services is measured indirectly by estimating output growth to equal input growth, and productivity for these services is assumed to stay the same.
As a result, we produce a separate productivity measure for directly measured services only, which, in FYE 2019, consists of residential and nursing care, and short-term care to maximise independence. This directly measured services productivity measure covered 37% of services by spending in FYE 2019. Productivity for directly measured services fell by 1.6% in FYE 2019, following a fall of 1.8% in FYE 20182. Data for the productivity of directly measured services are available in the Reference Tables. In Section 6, we provide further analysis on the productivity of residential and nursing care, which account for around 90% of directly measured services by spending.
The quality adjustment is not available for years before FYE 2011, as this was the year that the NHS Digital ASC Survey, used for measuring the quality adjustment, was introduced.
Notes for: Productivity
- Growth rates for a single year are given as the growth between the stated year and previous year. For example, the growth figure for FYE 2019 is the growth measured between FYE 2018 and FYE 2019. Growth rates for a period of more than one year are given as the growth between the first and the last year in that period. For example, growth between FYE 1997 and FYE 2019 represents growth between the level of a series in FYE 1997 and its level in FYE 2019.
- Because of a change in how activity data was recorded for short-term care to maximise independence in FYE 2018, this category of provision is indirectly measured for FYE 2018, meaning that productivity for directly measured services in FYE 2018 relates only to residential and nursing care services.
3. Inputs
Inputs cover the labour, intermediate consumption of goods and services, and capital used by local authorities in providing adult social care (ASC) services, as well as inputs used in providing care purchased by local authorities from independent sector providers. Analysis of ASC inputs is useful to understand the changes in the resources used to provide ASC services.
Figure 2 shows that inputs grew by 1.3% in financial year ending (FYE) 2019. This was the fourth consecutive year of growth since FYE 2015, following a period between FYE 2010 and FYE 2015 which recorded five consecutive years of falling inputs.
Most of the growth in inputs over the course of the time series since FYE 1997 has derived from increases in inputs used by independent sector providers in providing care purchased by local authorities. In FYE 2019, this accounted for 1.1 percentage points (pp) out of the overall 1.3% growth, with the remaining 0.2pp of growth derived from the increase in the inputs used by local authorities in the provision of ASC services. FYE 2019 was the only year out of the past four during which inputs used by local authorities in the provision of ASC services had increased.
While the level of inputs in FYE 2019 is nearly 50% higher than in FYE 1997, most of this increase occurred between FYE 2002 and FYE 2006. The level of inputs in FYE 2019 was only 1.7% higher than in FYE 2006.
The volume of inputs used to provide ASC services is calculated by accounting for the effects of inflation on ASC expenditure, a process known as deflation. This allows the growth in the volume of inputs provided to be distinguished from changes in the costs of those inputs.
Figure 3 shows how changes in expenditure and inflation have affected inputs growth.
Figure 3: The volume of ASC inputs in FYE 2019 was nearly 50% higher than in FYE 1997
Input expenditure and inflation for public service adult social care inputs, England, financial year ending (FYE) 1997 to FYE 2019
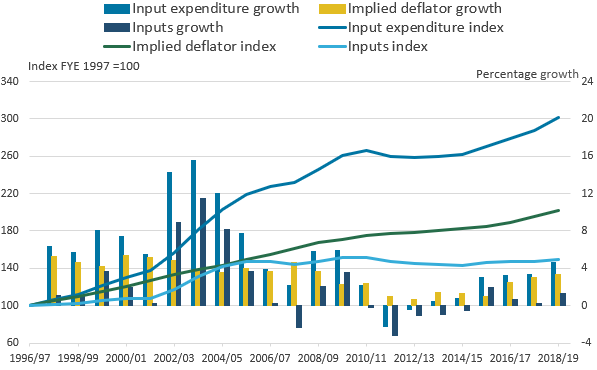
Source: Office for National Statistics
Notes:
- There is a change in the coverage of the series between FYE 2004 and FYE 2005 as NHS funding is included in the expenditure growth from FYE 2005 onwards. Because of the use of chain-linking, these changes do not result in a jump in the level of the expenditure index.
Download this image Figure 3: The volume of ASC inputs in FYE 2019 was nearly 50% higher than in FYE 1997
.png (24.6 kB) .xls (48.6 kB)Figure 3 shows that nearly three times more public expenditure was spent on ASC services in FYE 2019 than was spent in FYE 1997 in current prices. Over the same period, the cost of ASC inputs increased by 102%, meaning that the price level for ASC inputs approximately doubled. As a result, the quantity of inputs used in providing ASC rose by just under 50%.
Most of the trebling in expenditure over the series occurred between FYE 1997 and 2010, with little change occurring between FYE 2010 and 2015. However, while expenditure was stagnant during this period, inflation in input costs was also at its lowest rate over the series at this time, which limited the fall in ASC inputs.
Spending on adult social care services began to grow noticeably once again in FYE 2016, in part because of the introduction of the Better Care Fund. The Better Care Fund is a transfer from the NHS to local authorities that aims to improve efficiency and outcomes across health and social care by facilitating closer co-ordination between the two services.
Current price expenditure on ASC services increased at 3% or more per year each year since FYE 2016. However, this strong growth in expenditure is not mirrored in inputs growth, as input cost inflation also grew at a similar rate over the period. Overall input cost inflation reached 3.3% in FYE 2019, its highest rate since FYE 2009. Input cost inflation is analysed in more detail in Figures 4a and 4b.
In FYE 2019, local authority ASC labour cost inflation reached its highest rate in 10 years
While Figure 3 shows the overall effects of cost inflation on growth in inputs, Figures 4a and 4b break this down into the inputs deflators used to deflate labour and goods and services expenditure data respectively, to calculate ASC inputs. Faster growth in a deflator series means fewer inputs can be purchased for each pound of spending, and so higher deflator growth results in lower input growth for any given rate of spending growth.
Labour accounts for the majority of ASC inputs. Between FYE 1997 and FYE 2019, ASC labour costs roughly doubled, exceeding the increase in the costs associated with the intermediate consumption of goods and services.
Figure 4a: Independent sector labour cost inflation was around 4% in each of the last three years of the series
Deflators used in adult social care inputs, England, financial year ending (FYE) 1997 to FYE 2019
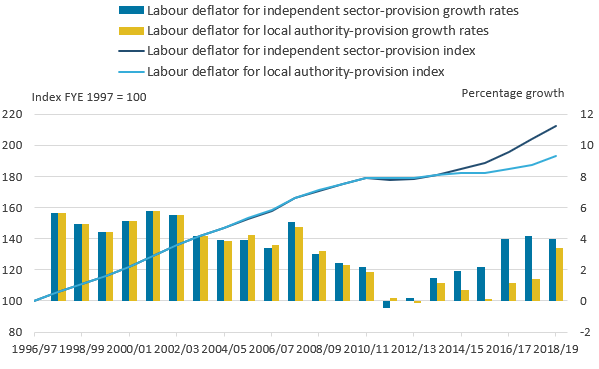
Source: Office for National Statistics, Department for Health and Social Care, Skills for Care
Download this image Figure 4a: Independent sector labour cost inflation was around 4% in each of the last three years of the series
.png (21.4 kB) .xls (49.7 kB)From FYE 2014 onwards, data from the National Minimum Dataset for Social Care (NMDS-SC) are used1 to estimate labour deflators for the local authority and independent sector separately. It should be noted that differences between the two series before FYE 2014 are only because of differences in the mix of staff groups employed in each sector, and so do not show the full difference between local authority and independent sector cost inflation.
Figure 4a shows that the labour costs of the two sectors have differed since the incorporation of NMDS-SC data into the deflators, with independent sector providers’ labour costs growing considerably faster than local authority costs up to FYE 2018. This may be the result of relatively large increases in the National Living Wage and National Minimum Wage since October 2014, as independent sector providers are more likely to employ staff at the minimum wage. The difference in labour costs was less pronounced in FYE 2019, with local authority costs growing by 3.4%, compared with growth of 1.4% the year before. Much of the rise in local authority labour costs in FYE 2019 are because of increases in the pay of managers and care workers.
Data from Skills for Care in 2016 (PDF, 439.58KB) and Skills for Care in 2019 (PDF, 903.39KB) show that for recent years, around two-fifths of care workers in the independent sector have been paid less than the subsequent year’s National Living Wage, compared with around 1% of local authority sector workers overall. This means that the effect of changes in the National Living Wage are likely to be smaller for local authority care workers.
Figure 4b: Inflation in intermediate consumption costs accelerated in the last three years of the series
Goods and services deflators used in adult social care inputs, England, financial year ending (FYE) 1997 to FYE 2019
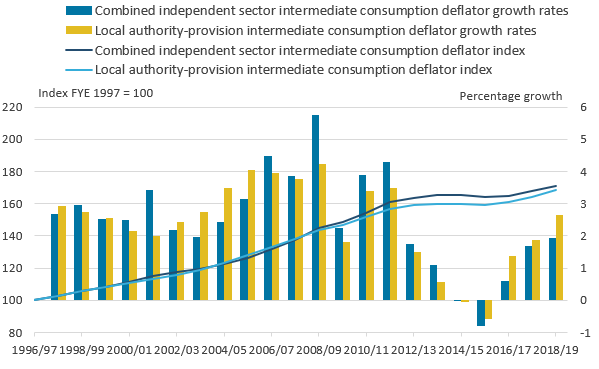
Source: Office for National Statistics, LaingBuisson, UK Home Care Association, Ministry for Housing, Communities and Local Government
Download this image Figure 4b: Inflation in intermediate consumption costs accelerated in the last three years of the series
.png (25.4 kB) .xls (47.1 kB)Deflators for the intermediate consumption of goods and services (Figure 4b) are produced using data from a range of sources. Data on what care providers spend on different types of goods and services inputs, such as utilities, transport, insurance, food and laundry services come from LaingBuisson, the UK Home Care Association and the Ministry of Housing, Communities and Local Government (MHCLG). A range of Office for National Statistics (ONS) price data are then used to provide appropriate deflators for each type of goods and services input.
Figure 4b shows that intermediate consumption cost inflation has generally been similar for local authority and independent sector providers. It should be noted that this is partly because both sets of intermediate consumption deflators rely on data for price growth observed in the general economy for the sorts of goods and services inputs used in ASC.
Figure 4c shows that, while the overall cost of ASC inputs (both labour and non-labour) over the period FYE 1997 to FYE 2019 doubled, prices in the general economy, measured using the gross domestic product (GDP) deflator, only increased by 49%. This divergence was mainly because ASC labour cost inflation exceeded growth of the GDP deflator before FYE 2012.
Figure 4c: ASC input cost inflation grew considerably faster than general economy inflation for most of the series
Implied deflators for adult social care inputs and the overall economy, England, financial year ending (FYE) 1997 to FYE 2019
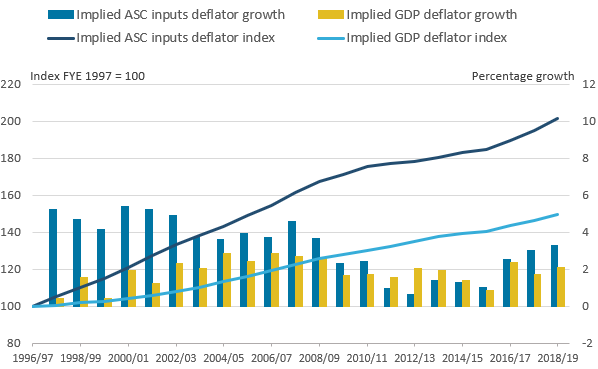
Source: Office for National Statistics, Department for Health and Social Care, Skills for Care, LaingBuisson, UK Home Care Association, Ministry for Housing, Communities and Local Government, LondonADASS Improvement Programme
Download this image Figure 4c: ASC input cost inflation grew considerably faster than general economy inflation for most of the series
.png (23.5 kB) .xls (41.5 kB)After a period between FYE 2011 and FYE 2017 when ASC input cost inflation was lower than or similar to the GDP deflator, ASC input cost inflation returned to growing substantially faster than general economy inflation in FYE 2018 and FYE 2019. In FYE 2019, the GDP deflator grew by 2.1%, while the ASC input cost deflator grew by 3.3%. This indicates greater cost pressures in the ASC sector than the overall economy, largely caused by ASC wage growth.
More information on the deflators used in the inputs can be found in the Public service productivity: adult social care, sources and methods, 2019 update, while further breakdowns of these deflators are available in the Reference Tables.
Notes for: Inputs
- As with other breaks in series used in the productivity measure, the use of chain-linking means this change does not result in a step-change in the deflators.
4. Output quantity
Output quantity relates to the amount of adult social care (ASC) services provided in a given year. Figure 5 shows that the quantity of publicly funded ASC services provided grew by 0.9% in FYE 2019, and was around 31% higher than in FYE 1997. It is important to note that these figures differ from those used to calculate productivity in Section 2, as they do not adjust output to account for the quality of services provided. For more information on quality adjusted output, see Section 5.
Figure 5: In FYE 2019, quantity output was at largely at the same level as in FYE 2013
Public service adult social care non-quality adjusted output, England, financial year ending (FYE) 1997 to FYE 2019
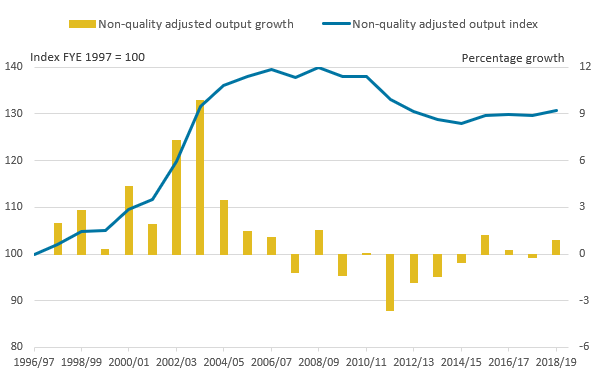
Source: Office for National Statistics
Download this image Figure 5: In FYE 2019, quantity output was at largely at the same level as in FYE 2013
.png (17.0 kB) .xls (39.4 kB)The increase in ASC quantity output over this period can be divided into several distinct phases:
- FYE 1997 to FYE 2007, where quantity output increased in each year, rising by 40% over the period
- FYE 2007 to FYE 2011, during which quantity output was largely unchanged
- FYE 2011 to FYE 2015, where quantity output fell by 7.2% over the period
- FYE 2015 to FYE 2019, during which quantity output increased by 2.1% overall, largely because of increases in FYE 2016 (the year the Better Care Fund was introduced) and FYE 2019
It is important to remember the overall context of changing care needs during the period when analysing changes in the volume of output produced, although limitations in the data available mean this is challenging. One option is to analyse the change in population over the period. During the period 1996 to 2018, the number of people aged over 64 years in England rose by 32%, while the number of people aged 85 years and over grew by 57%. As care needs generally increase with age, people aged 85 years are more likely to require ASC assistance than people aged 65 years1, which implies there is likely to have been an increase in demand for adult social care services for older people over this period.
However, it is important to note that over half of ASC expenditure that is attributable to a specific age group is on working-age adults (those aged between 18 and 64 years). Working-age adults requiring ASC services generally have different needs to older adults, with support for adults with learning disabilities accounting for most ASC expenditure on working-age adults.
While the population aged between 18 and 64 years grew by only 19% between 1996 and 2018, figures from Public Health England (PDF, 1.21MB) on patients registered with their GP as having a learning disability have risen in recent years from 139,000 in FYE 2007 to 214,000 in FYE 2014. This indicates an increase in care needs for the working-age group beyond population growth, although this rise may be partly because of improvements in GP recording. Emerson and Hatton (2011) (PDF, 986KB) project that changes in the provision of ASC services for adults with learning disabilities will have to grow by between 1.2% and 5.1% in the 18 years up to 2030, which is above the rate of general population growth.
It is important to remember that public service productivity statistics only relate to publicly funded ASC services, so exclude privately funded care and unpaid care provided by family members, friends and volunteers. Furthermore, the measure excludes services funded through client contributions to local authority services, which are determined through the use of personal wealth thresholds. This means that output in our measure will be affected by the wealth of people in need of care.
Our UK Health Accounts provide data on total long-term care spending across the whole economy, including private spending. While these data do not exactly match the coverage of ASC services included in the productivity analysis2, they show that non-government financing of long-term care increased by 18.2% between 2013 and 2017 (from £15.7 billion to £18.5 billion), relative to public expenditure which increased by 12.6% (from £26.3 billion to £29.7 billion).
Data from the Household satellite account suggest the total number of informal care hours received by adults rose from 6.4 billion in 2005 to 8.5 billion in 2013, before falling back to 7.9 billion in 2016. It should be noted that these figures mainly include hours of continuous care for people who require the constant presence of a carer, and only a small proportion of the total hours received relate to personal and practical care that many ASC home care services provide.
Therefore, while these figures suggest that an increase in non-government funding of services may be meeting some of the growing need for care, there is little apparent growth in unpaid care and we cannot confirm that non-government funding or unpaid sources account for the apparent difference in growth between publicly funded ASC output and care needs.
In FYE 2019, output growth was driven by indirectly measured services, such as supported living
For services where activity data are available, the quantity of ASC output is measured “directly”, by calculating the growth rates of different adult social care (ASC) activities and weighting these by their unit costs. As a result, growth in activities that are common and expensive has a greater effect on the output index than a similar rate of growth in activities that are uncommon and low-cost. For services where activity data are not available, output growth is measured “indirectly” on the “output-equals-inputs” basis, by assuming output growth to be equal to inputs growth.
Figure 6 shows how directly and indirectly measured services have driven changes in publicly funded ASC output over the series. More information on how output growth is calculated can be found in Section 9 and Public service productivity: adult social care, sources and methods, 2019 update.
Figure 6: Residential and nursing services made a negative contribution to output in every year since FYE 2005
Contributions to public service adult social care output growth, England, financial year ending (FYE) 1998 to FYE 2019
Source: Office for National Statistics
Notes:
- Expenditure on direct payments was first separately recorded in the data in FYE 2001.
- There is a break in series between FYE 2014 and FYE 2015 because of a change in data collection, resulting in most community services being measured indirectly from FYE 2015 on.
- Up until FYE 2014, other directly-measured provision included home care, day care, referrals and assessments, meals, as well as equipment and adaptations. From FYE 2015, this category includes only short-term care to maximise independence.
- Because of a change in how activity data were recorded for short-term care to maximise independence in FYE 2018, this category of provision is indirectly measured for FYE 2018, but directly measured in FYE 2019.
Download this chart Figure 6: Residential and nursing services made a negative contribution to output in every year since FYE 2005
Image .csv .xlsThe main component of directly measured services in FYE 2019 was residential and nursing care, which has made a negative contribution to the change in output in every year measured since FYE 2005. Prior to this, most residential and nursing care contributions to output growth were positive.
Residential and nursing care services are the only form of ASC that has been measured directly since the series began in FYE 1997. Other indirectly measured services have varied, depending on available activity data. Up until FYE 2015, a range of community care services including home care and day care were directly measured, as well as referrals to local authority social care services and assessments to determine what care would be appropriate for clients. However, in FYE 2019 short-term care to maximise independence was the only service directly measured in addition to residential and nursing care.
It should be noted that because of a change in data collections between FYE 2014 and FYE 2015, it is not possible to analyse the contributions of individual service types to ASC output growth between these two years, with total output growth measured on the “output-equals-inputs” basis.
| England | Percentage points | |||
|---|---|---|---|---|
| FYE 2016 | FYE 2017 | FYE 2018 | FYE 2019 | |
| Residential & nursing care | -0.6 | -0.2 | -0.6 | -0.1 |
| Other directly measured services | -0.2 | -0.2 | 0.0 | 0.2 |
| Direct payments¹ | 0.9 | 0.3 | 0.1 | 0.0 |
| Supported living¹ | 0.1 | 0.7 | 0.7 | 1.0 |
| Home care¹ | -0.1 | -0.1 | 0.0 | -0.1 |
| Other¹ | 1.1 | -0.2 | -0.5 | 0.0 |
Download this table Table 1: Contributions to public service adult social care output growth, financial year ending (FYE) 2016 to FYE 2019
.xls .csvTable 1 expands the analysis in Figure 6 to provide a more granular breakdown of contributions to output growth since the FYE 2015 series break. These figures include rough estimates for the contribution to output growth from indirectly measured services, although it should be noted that, with the exception of residential and nursing care, other directly measured services, and direct payments, these estimates are based on non-service-specific deflators.
Table 1 shows a large contribution to output growth in FYE 2019 from supported living services, which also provided large contributions to output growth in preceding years. Over the same period, residential and nursing care output has fallen, which may point to councils erring towards the use of services where the accommodation element will be largely covered by Housing Benefit payments, rather than utilising local government funding, as suggested in an article by LaingBuisson.
Direct payments involve local authorities providing funding to care clients to enable them to arrange and pay for the care themselves, in place of the local authority commissioning the care for them. This often enables clients to receive a more personalised service tailored to their needs. Prior to FYE 2019, output growth for direct payments increased in each year in which they have been recorded over the series, but this growth rate has slowed in recent years and direct payments did not contribute to output growth in FYE 2019. The King’s Fund (PDF, 969KB) reports that growth in the number of service users receiving direct payments has also stalled in recent years, but the reasons behind this slowdown are not fully understood.
Notes for: Output quantity
- More information on how care needs change with age is available from the English Longitudinal Study on Ageing.
- Long-term care expenditure accounts for services aimed at managing chronic health conditions related to long-term care dependency (including old-age and disability-related conditions) and reducing suffering where an improvement in health is not expected. This covers most ASC expenditure, but has a wider definition than ASC, while some ASC services, such as drug rehabilitation, are not included in long-term care expenditure in the health accounts.
5. Output quality
Output can also be adjusted to take into consideration changes in the quality of the services provided. Quality-adjusted output growth is used to measure productivity growth in Section 2. The quality adjustment to adult social care (ASC) output is based on the concept of adjusted social care-related quality of life and produced using data from the Adult Social Care Survey (ASCS).
The quality adjustment measures changes in how well care clients’ needs are met across domains of quality of life that are affected by social care1, while taking into account factors outside the control of ASC services which may also affect quality of life. This allows the changes in care clients’ quality of life which are the result of changes in the quality of local authority-provided or arranged ASC services to be measured. More information on the methodology behind the quality adjustment is available in Public service productivity: adult social care, sources and methods, 2019 update.
The ASCS data used to produce the quality adjustment are only available from financial year ending (FYE) 2011 onwards, and output before this cannot be quality adjusted. Furthermore, a change to the ASCS between FYE 2014 and FYE 2015 means that no quality change can be calculated for FYE 2015.
Figures derived from the ASCS for changes in the quality of ASC services should be regarded as estimates because of the nature of data collection in this sample survey. Issues related to use of the ASCS are discussed in Section 9.
Figure 7 shows that before applying a quality adjustment, output fell by 5.3% between FYE 2011 and FYE 2019. However, when accounting for the increase in the quality of services provided, output fell by 1.7%. For the first five years in which quality was measured, the quality adjustment was positive, resulting in an increase to output, but the change in quality was negative in FYE 2018 and FYE 2019, decreasing output. In FYE 2018 this was coupled with a decrease in the quantity of output provided, whereas in FYE 2019 the fall in quality offset an increase in the quantity of output.
Figure 7: Quality adjustment has had a positive contribution to output, except in FYE 2018 and FYE 2019
Output quality adjustment, England, financial year ending (FYE) 2011 to FYE 2019
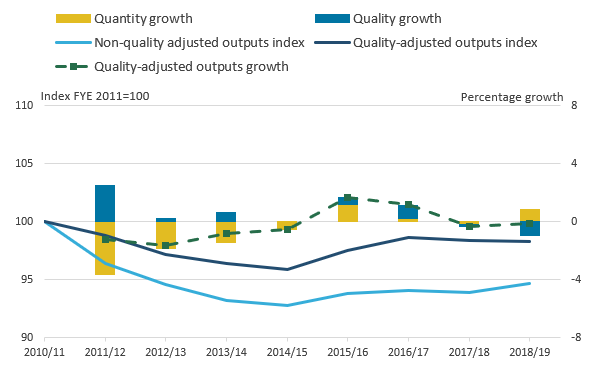
Source: Office for National Statistics
Notes:
- Quality growth is not estimated for FYE 2015 because of a break in series.
Download this image Figure 7: Quality adjustment has had a positive contribution to output, except in FYE 2018 and FYE 2019
.png (20.0 kB) .xls (50.2 kB)
| England | Percentage growth | |||||||
|---|---|---|---|---|---|---|---|---|
| FYE 2012 | FYE 2013 | FYE 2014 | FYE 2015 | FYE 2016 | FYE 2017 | FYE 2018 | FYE 2019 | |
| Overall quality adjustment | 2.5 | 0.2 | 0.7 | 0.0 | 0.5 | 0.9 | -0.1 | -1.0 |
| Residential and nursing care – all adults | 0.7 | 0.1 | -0.6 | 0.0 | 0.6 | 0.3 | -0.4 | -0.6 |
| Community care - all adults | 3.9 | 0.4 | 1.7 | 0.0 | 0.4 | 1.4 | 0.1 | -1.2 |
| All social care - older adults | 1.8 | 0.8 | 0.0 | 0.0 | 0.0 | 1.1 | 0.0 | -0.2 |
| All social care - working age adults | 3.1 | -0.2 | 1.2 | 0.0 | 0.9 | 0.8 | -0.2 | -1.6 |
Download this table Table 2: Growth in components of adult social care output quality adjustment, financial year ending (FYE) 2012 to FYE 2019
.xls .csvIn FYE 2019, the quality adjustment fell for residential and nursing care, and community care, particularly for clients with learning disabilities. However, the fall in quality was greater in community care.
Despite falls in quality in FYE 2019, overall, the quality adjustment reduced the fall in output between FYE 2011 and FYE 2019 from 5.3% to 1.7%. The positive effect of the quality adjustment on output indicates an increase in social care-related quality of life attributable to improved ASC service quality, although this should be interpreted with regard to the caveats highlighted in Section 9.
When output is adjusted for quality, productivity fell by 0.2% between FYE 2011 and FYE 2019, however, without the quality adjustment it fell by 3.8%.
While Figure 7 shows the effects of the quality adjustment on output, Figure 8 brings together adult social care (ASC) inputs and output quantity and quality for the period FYE 2011 to FYE 2019, the years for which the quality adjustment is available.
Figure 8: Quality adjustment reduced the fall in productivity, except for the latest two years
Public service adult social care productivity, quality and non-quality adjusted, England, financial year ending (FYE) 1997 to FYE 2019
Source: Office for National Statistics
Notes:
- No productivity change is calculated for FYE 2015 because of a change of data source between this and the previous year.
Download this image Figure 8: Quality adjustment reduced the fall in productivity, except for the latest two years
.png (18.7 kB) .xls (50.2 kB)When output is not adjusted for quality, ASC productivity is shown to have fallen over the period by 3.8%. However, if the change in quality of output is taken into consideration, productivity fell by just 0.2% over the same period. While the effects of the quality adjustment over the whole period have reduced the fall in productivity, the fall in output quality in FYE 2019 had the effect of reducing productivity further. In FYE 2019, productivity unadjusted for the quality of output fell by 0.4%, but this was increased to a fall of 1.4% when the quality of output was taken into consideration.
Notes for: Output quality
- The domains of quality of life used are those identified in the Adult Social Care Outcomes Toolkit (ASCOT): control, personal care, food and nutrition, accommodation, safety, social participation, occupation, dignity.
6. Productivity in residential and nursing care
While using both directly and indirectly measured output is necessary to ensure total output growth can be measured, the inclusion of indirectly measured output can reduce the scale of changes in the overall productivity measure. For example, where productivity is falling for both directly and indirectly measured services, but this fall can only be measured for directly measured services, the inclusion of indirectly measured output would result in an underestimation of the fall in productivity. This section analyses the main component of directly measured services – residential and nursing care – excluding the dampening effect of indirectly measured services.
As noted in Section 4, where activity data are available, these are weighted by their costs to produce directly measured output. Directly measured output is preferred to that which is indirectly measured, as it enables the calculation of productivity change.
In FYE 2019, almost all directly measured output related to residential and nursing care1. This is also the only service type that is measured directly throughout the whole series, with the exception of FYE 2015, when there was a change in data collection and all output was indirectly measured. Residential and nursing care output is measured by the number of weeks of care provided, with separate weights given to different client age and support need groups, to account for differences in the cost of providing care to different groups of clients.
Services provided in residential and nursing care settings accounted for around one-third of adult social care (ASC) spending in FYE 2019 (Figure 9). This is down from around 45% of adult social care expenditure in FYE 1997. The King’s Fund (PDF, 969KB) notes that home-based care is often preferable for clients and typically requires less expenditure than residential and nursing care, which may help to explain the fall in spending on residential and nursing care as a share of ASC services. In addition, the Personal Social Services Research Unit (PDF, 333.11KB) report that the introduction of personal budgets, in particular, is seen as a means of placing the client and their family at the centre of the decision-making regarding their care needs, and as a more cost-effective form of care from the perspective of care-related quality of life.
Figure 9: Expenditure on residential and nursing care accounted for around one-third of public ASC spending in FYE 2019
Percentage of public adult social care expenditure on residential and nursing care, England, financial year ending (FYE) 1997 to FYE 2019
Source: Office for National Statistics
Notes:
- There is a break in series between FYE 2014 and FYE 2015 because of a change of data collection.
Download this chart Figure 9: Expenditure on residential and nursing care accounted for around one-third of public ASC spending in FYE 2019
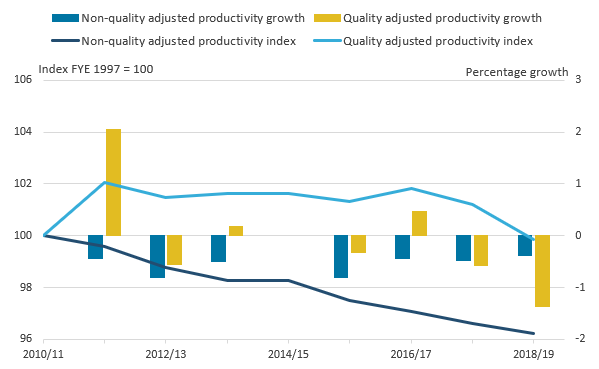
Image .csv .xlsResidential and nursing care productivity fell by 2.2% in FYE 2019, the fourth consecutive year of falling productivity
Residential and nursing care productivity fell by 2.2% in FYE 2019, continuing the trend of falling productivity in the financial years ending 2016, 2017 and 2018. The fall in productivity in FYE 2019 was a result of inputs growing and output decreasing. A fall in the quantity of output produced was exacerbated by a decline in the quality of services provided.
Further discussion on why productivity may have fallen is available in Section 2.
Figure 10: The quantity of residential and nursing care services provided in FYE 2019 was lower than in FYE 1997, despite higher inputs
Public service residential and nursing care; inputs, and quality adjusted and non-quality adjusted output and productivity, England, financial year ending (FYE) 1997 to FYE 2019
Source: Office for National Statistics
Notes:
- No productivity change is calculated for FYE 2015 because of a change of data source between this and the previous year.
Download this chart Figure 10: The quantity of residential and nursing care services provided in FYE 2019 was lower than in FYE 1997, despite higher inputs
Image .csv .xlsIn FYE 2019, non-quality adjusted residential and nursing care productivity fell by 1.6%. Including the quality adjustment resulted in the fall increasing to 2.2%. This reflects the negative effect of quality in FYE 2019 on output, where non-quality adjusted output fell by 0.4%, but after including changes in quality, output fell by 1.0%. Productivity fell in both instances, as alongside the fall in output, inputs increased.
The quantity of output produced also fell in FYE 2016 to FYE 2018. In FYE 2016 and FYE 2017 this fall in activity was partially offset by increases in the quality of services provided, but in FYE 2018 the quality of output produced also fell, as in FYE 2019.
In FYE 2019, the quantity of residential and nursing care services provided was 1.7% lower than in FYE 1997. Over the same period, the amount of inputs used was 20.2% higher in FYE 2019 compared with FYE 1997. The overall impact of the quality adjustment on residential and nursing care productivity has been minor, with productivity at the same level in FYE 2019 relative to FYE 1997 whether quality adjusted or non-quality adjusted.
Notes for: Productivity in residential and nursing care
- In FYE 2019, 91% of directly measured output was residential and nursing care, and 9% short-term care.
7. Productivity by client age group
This section analyses the productivity of adult social care (ASC) services by the two main client age group classifications used by NHS Digital: working-age clients (those aged 18 to 64 years) and older clients (those aged 65 years and over). For comparability, both series measure only services for which activity data are available1, because of the methodological issues mentioned in Section 6.
The reasons why older and working-age clients need social care support are often different. In FYE 2019, the majority of spending on services for older adults was to provide support for physical disabilities, whereas the majority of spending on services for working-age adults was to provide support for learning disabilities.
Productivity has fallen for ASC services for both age groups over the period FYE 1997 to FYE 2019, although it has fallen more for working-age clients’ services (Figure 11). The fall in productivity for older adults’ services is partly because of a fall in output and an increase in inputs, whereas for working-age clients’ services, both inputs and output grew over the period, but growth in inputs was stronger.
Between FYE 2011 and FYE 2018, this pattern reversed, with productivity levels falling less for working-age clients’ services. During this period, both inputs and output fell for services for working-age clients, but the fall in output was slightly larger. The quality adjustment over this period has had an overall positive effect on the change in output, with the overall effect greater for working-age clients’ services.
Figure 11: Over the whole time series, the productivity of working-age adults’ care fell by more than older adults’ care
Quality and non-quality adjusted productivity for older adult and working age adult services, directly-measured ASC services only, England, financial year ending (FYE) 1997 to FYE 2019
Source: Office for National Statistics
Notes:
- No productivity change is calculated for FYE 2015 because of a change of data source between this and the previous year.
Download this chart Figure 11: Over the whole time series, the productivity of working-age adults’ care fell by more than older adults’ care
Image .csv .xlsHowever, in FYE 2019, productivity in services for working-age adults fell by 2.0% compared with 1.4% in services for older clients. The productivity fall for working-age adults in FYE 2019 was driven by a decrease in the quality of output, particularly for clients with learning disabilities, which represents the majority of spending on working-age clients. By contrast, the fall in productivity in services for older adults was mostly driven by the volume of inputs used increasing at a faster rate than the amount of output provided.
It should be noted that the same deflators are applied to the inputs for both age groups and this may be a source of some of the difference in these productivity series, as the higher cost of services for adults with learning disabilities is partly because of their more labour-intensive nature.
Notes for: Productivity by client age group
- Services for which output is measured directly and by age band are: residential and nursing care for the whole series; day care and referrals and assessments until FYE 2014; and short-term care to maximise independence from FYE 2015 to FYE 2017 and in FYE 2019.
8. Revisions
Figure 12 shows how the adult social care (ASC) productivity series has been revised since the last edition, Public service productivity: adult social care, England, financial year ending 2018.
Figure 12: Productivity growth was revised by no more than 0.1 percentage points in any given year
Revisions to public service adult social care productivity, England, financial year ending (FYE) 1997 to FYE 2019
Source: Office for National Statistics
Notes:
- No productivity change is calculated for FYE 2015 because of a change of data source between this and the previous year. 2. Quality adjustment applies after FYE 2011.
Download this image Figure 12: Productivity growth was revised by no more than 0.1 percentage points in any given year
.png (25.2 kB) .xls (52.7 kB)Productivity growth was revised by no more than 0.1 percentage points in any given year, when comparing with figures published in last year’s bulletin.
There are two main sources of revisions in the data.
Firstly, estimates of local authority capital consumption in the inputs incorporate methodological improvements to the estimation of this element in the national accounts, including a review of asset lives. These data reflect changes that were included in Blue Book 2019. These changes result in inputs growth being revised down and therefore productivity growth being revised up.
Secondly, the deflators used in independent sector intermediate consumption have been revised using updated expenditure data from LaingBuisson and the UK Home Care Association. The ratio of the cost of intermediate goods and services to labour for independent sector-provided services was also revised using these more recent data.
While these changes mainly affect ASC inputs, they will also revise estimates of ASC output, as a share of output is measured indirectly through the “output-equals-inputs” approach.
Nôl i'r tabl cynnwys9. Quality and methodology
How do we measure productivity?
Public service productivity is estimated by comparing growth in the total quantity of inputs used with growth in the total quantity of output provided, adjusted for the quality of this output. If the growth rate of output exceeds the growth rate of inputs, productivity increases, meaning that more output is being provided for each unit of input. Conversely, if the growth rate of inputs exceeds the growth rate of output, then public service productivity will fall, indicating that less output is being provided for each unit of input.
Inputs are composed of labour, goods and services, and capital consumption, and are measured on a volume basis using expenditure adjusted for the specific input cost inflation rates faced by adult social care (ASC) services.
Quantity output is measured as the number of individual activities performed weighted by their cost, where activity data are available. Where activity data are not available, output is measured using the equivalent deflated expenditure data as inputs. A quality adjustment is applied to output to account for changes in service quality.
While these productivity estimates provide a measure of the amount of output that is provided for each unit of input, they do not measure value for money, whether inputs have been obtained for the lowest possible cost, or whether most appropriate forms of care have been used.
What do we mean by adult social care?
This publication focuses on adult social care (ASC). ASC services provide care and support to adults with learning or physical disabilities, adults with mental health problems, drug and alcohol misusers, and carers. ASC services include:
- placements in residential and nursing care
- provision of home care services
- day care services
- supported living and accommodation
- “Meals on wheels”
- equipment and home adaptions
- care assessments and support services
What do we mean by public service?
The term “public service” is used, as this publication only covers publicly funded ASC services, with public funding covering both local authority funding and contributions from the NHS (from financial year ending (FYE) 2005 onwards). Privately funded ASC services are excluded from input, outputs and productivity. However, publicly funded services provided by independent sector providers are included.
How have data sources changed over time?
There have been several changes in the data sources over time:
- Data on funding for social care received by local authorities from the NHS was not available prior to FYE 2005; local authority-provided or -arranged social care activity funded by the NHS is only incorporated in the growth of inputs and output from FYE 2005 onwards.
- The source for the quality adjustment, the Adult Social Care Survey, was introduced in FYE 2011, and so the quality adjustment is first applied to output growth between the years FYE 2011 and FYE 2012.
- There was a change in how social care data were collected between FYE 2014 and FYE 2015 which affected financial, activity, and quality data; as a result, changes in productivity and the quality adjustment cannot be measured, and output is assumed to grow at the same rate as inputs between these two years.
- From FYE 2014 onwards, activity data are not available for referrals and assessments and community care services, such as home care and day care and so output is assumed to be equal to inputs, and productivity changes cannot be estimated after FYE 2014 for these services.
- A change in the unit of activity used to record short-term care to maximise independence between FYE 2017 and FYE 2018 meant that changes in the productivity of short-term care could not be measured between these years; as two consecutive years of the new activity data exist for FYE 2018 and FYE 2019, this can once more be directly measured output.
Because of the use of chain-linking to produce input and output indices, these changes do not result in a jump in the level of input and output indices. The chain-linking methodology used to construct the output and inputs indices means that the indices are constructed from a series of growth rates between consecutive pairs of years. As a result, where there are changes in how some of the data are reported, these do not result in step-changes in the level of inputs or output. More information can be found in Methodology Notes: Annual chain-linking (PDF, 58.02KB).
What data quality issues should users be aware of?
As noted in Section 5, the quality adjustment is produced using data from a sample survey – the Adult Social Care Survey (ASCS) – and figures produced from this survey should be regarded as estimates. As detailed in the Data quality report for the ASCS (PDF, 676KB), users of this data should be aware of several issues affecting the data.
Firstly, as users selected to complete the ASCS are not compelled to do so, the size of the sample of users achieved by the ASCS is much lower than the sample originally selected. In recent years, response rates have fallen to around 32%. If there are systematic differences in the perceived quality of care between those who choose to complete the survey and those who do not, the results could be biased.
Another issue is that, to enable the survey to be representative of as many care users as possible, care users are permitted to receive help in completing the survey. Where necessary, help from friends or family members is recommended, but help from care workers is also permitted, and respondents receiving help from care workers account for around a quarter of the total. This may introduce a further bias into the data, as analysis of the data carried out by NHS Digital suggests respondents report higher quality of life when completing the survey with the support of a care worker.
Furthermore, as the survey is administered by local authorities directly, there are some variations in how it is administered. NHS Digital reports instances where local authorities have deviated from the survey guidance in its Data Quality Statement.
How does this report relate to the UK National Accounts?
While much of the data used in the measure are also used in the production of the national accounts, methodological changes mean that ASC output in this publication is different to the national accounts. Recent data source and relevant methods changes made to produce this article will be incorporated into the national accounts in the future.
Where can I find further information about the methodology used?
Public service productivity: adult social care, current method, 2019 update provides a detailed description of the methodology used, and the Public service productivity: adult social care QMI provides an overview of the measures, and more information about their strengths and weaknesses.
Nôl i'r tabl cynnwys